Definition of Hernia
A hernia is a protrusion of viscera through its peritoneal covering. This differentiates a hernia from a prolapse, in which inner organs without a peritoneal covering protrude, e.g. the rectum. External hernias such as inguinal or femoral hernias can be distinguished from internal hernias. The latter protrude e.g. through existing gaps in diaphragm muscle or through defects in the mesentery secondary to surgery. The causes of herniation include congenital and acquired connective tissue defects as well as scars.
Inguinal hernia
Congenital inguinal hernias can be distinguished from those that are acquired. The anatomic landmarks that distinguish the two types from one another are the epigastric vessels. Hernial orifices running medial of the epigastric vessels cause direct inguinal hernias, which are always acquired. Lateral to the epigastric vessels indirect inguinal hernias pass through the inguinal canal. They arise from incomplete adhesion of the vaginal process, and
are therefore always congenital. The inguinal canal is formed by several anatomic structures, exact knowledge of which makes possible any understanding or surgical treatment of inguinal hernias. The floor of the inguinal canal is formed by the inguinal ligament, the anterior wall (Vorderwand) by the aponeurosis of the external oblique muscle. The roof is formed by the lower margin of the (Unterrand) internal oblique muscle and the transverse abdominis muscle. The posterior wall of the inguinal canal is formed by the transversalis fascia.
In males, the inguinal canal contains the ductus deferens, testicular artery, artery to ductus deferens, pampiniform plexus, cremaster muscle, Ramus genitalis of the genitofemoral nerve, and sympathic nerve fibers. In women, the ligamentum rotundum or ligamentum teres uteri run through the inguinal canal.
A recent publication by Hutan Ashrafian of the Imperial College in London discusses the possibility that an inguinal hernia is visible slightly above the left side of the groin of Leonardo da Vinci’s Vitruvian Man.
Symptoms
Inguinal hernias cause pain in the groin and a feeling of pressure or heaviness. The extent of the complaints gives no indication of the size of the hernia. Clinically a distinction is made between reducible, irreducible, and incarcerated inguinal hernias. In the latter, intestinal arteries trapped in the hernial sac are compressed and ischemia and necrosis threaten. In such cases, emergency surgery is always indicated.
Diagnosis & Clinical Management
Diagnosis of an inguinal hernia is made clinically, i.e. without the use of equipment-based procedures. Sonography serves only to confirm or exclude differential diagnoses such as testicular torsion.
In males, the hernial orifices on both sides are examined with the patient in a standing position. Using the forefinger, the abdomen is palpated from the scrotum toward the deep inguinal ring, which should be just passable with the tip of the forefinger. The patient is asked to cough or press down. If an inguinal hernia is presence, a slight bulging might be felt.
Large hernias are visible to the naked eye. In such cases, an attempt can be made to reduce the herniated tissue manually with the patient lying in a supine position.
In hernias with prolonged strangulation, the trapped bowel segments may well suffer ischemic injury with consequent risk of perforation. After manual reduction in such cases, therefore, the patient should be admitted to hospital. Also feared is so-called en masse reduction, in which complete reduction of the hernia contents appears successful, whereas in fact the hernial opening including the neck have only been repositioned and the strangulated obstruction remains.
Operation
Various procedures are available for surgical repair of inguinal hernias. In addition to open procedures, minimally invasive techniques are seeing increasing use. A further distinction is made between suture and mesh procedures. In suture procedures, the anatomic weak point that gave rise to the hernia is strengthened by doubling of the fascia. In mesh procedures, partially resorbable synthetic meshes create stability by providing a scaffold for new tissue growth. Meshes are used in both endoscopic and open procedures.
Which OP procedure is optimal depends on many factors, among them the patient’s age and possible risk factors, but also on whether the hernia is primary or recurrent.
Shouldice Repair
In this open suture procedure, the posterior wall of the inguinal canal, the transverse fascia, is split, doubled over on itself, and sutured. The internal oblique muscle and the transverse abdominal muscle are sutured to the inguinal ligament. This second step is performed analogously to the Bassini repair, which has been largely abandoned in favor of the Shouldice technique.
Transabdominal Preperitoneal Plasty (TAPP)
A synthetic mesh can also be placed intraperitoneally in the inguinal canal. Using a transabdominal minimally-invasive access, a peritoneal window is created, the mesh placed behind (hinter) the transverse fascia and the peritoneum closed again. This method has the advantage that the contralateral side can also be evaluated without additional incisions and surgically repaired if needed.
This access is also available in case of recurrence after open inguinal herniotomy.
Total Extraperitoneal Plasty (TEP)
To avoid creation of intra-abdominal adhesions or injuries, the procedure is performed in an artificial space between the abdominal wall and peritoneum. The space is created by dissection with a balloon trocar and although it offers a less than ideal view, the risk of mesh slippage is lower. The contralateral side can also be inspected and repaired.
OR-Video: Lichtenstein Repair, open herniotomy with mesh placement (Netzeinlage)
1 Access
The skin incision is made over the inguinal canal..
- Dissection through the subcutaneous fat tissue
- Subcutaneous veins are ligated and severed
- The external aponeurosis is exposed
- From it the superficial inguinal ring is exposed
2 Exposure of the Inguinal Canal
- The inguinal canal is exposed
- In this case, the ilioinguinal nerve is located directly on the hernial sac
- It is infiltrated with local anesthetic and severed
- Neurectomy is indicated in this case because otherwise there is a risk of chronic groin pain
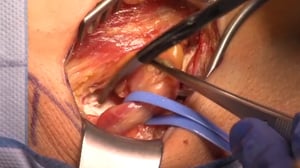
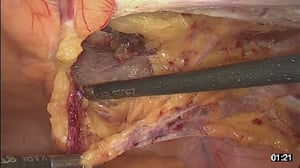
3 Dissection of the Hernial Sac
- The hernial sac is removed from the inguinal canal
- The superficial inguinal ring is severed
- The inguinal canal structures are snared with a string
- This patient has an indirect inguinal hernia
- The hernia is filled with preperitoneal fat
- The hernial contents are reduced, the hernial orifice closed
4 Structures in the Inguinal Canal
In males, the following structures run though the inguinal canal:
- vas deferens (evident as a whitish cord in video)
- Cremaster muscle
- A. testicularis
- Pampiniform plexus
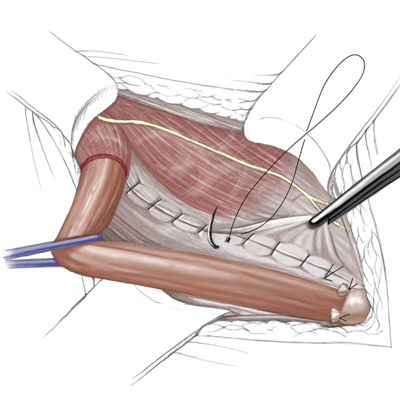
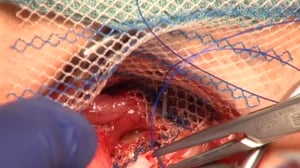
5 Mesh Placement
- The hernial orifice is covered with a partially resorbable mesh
- Starting at the symphysis, the mesh is attached with nonresorbable suture to the inguinal ligament
- To allow passage of inguinal canal structures, the mesh is incised in a dovetail-like shape
- The mesh is then affixed to the transverse fascia
6 Closure
- The external aponeurosis is closed
- Completing reconstruction of the inguinal canal
- An epifascial drain is placed
- Skin closure is done intracutaneously
- A staple patch is applied
OR-Video: TAPP, endoscopic inguinal hernia operationn
1 Access & Trocar placement
- A subumbilical incision is made for the optical trocar
- The anterior lamina of the rectus sheath is exposed and opened
- The peritoneum is incised
- Stay sutures are placed at the level of the fascia for attachment of the trocar. The fascia will later be closed with these sutures.
- The 10-mm optical trocar is inserted
- The capnoperitoneum is created
- Two additional 5 mm trocars are inserted
2 Incision of the Peritoneum
- A peritoneal window is created over the inguinal canal using electric scissors
- The peritoneum is resected exposing the structures of the inguinal canal
- The epigastric vessels separating medial from lateral inguinal hernias are easily identified
3 Dissection of the Hernial Sac
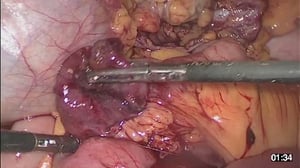
- Now the hernial sac is dissectedt
- Care is taken to spare the structures of the inguinal canal
- In this case, a direct, i.e. medial, inguinal hernia is present. The hernial sac is ligated with a loop (Schlinge) and removed.
4 Placement of the Mesh
- EA rolled-up, partially resorbable mesh is introduced into the site
- It is unrolled and placed in front of the hernial orifice
- It is affixed with fibrin glue. The blue coloring serves only to indicate where glue has already been applied
5 Closure of the Peritoneum
- When the mesh has been affixed, the peritoneum is closed again
- Using a special barbed thread. The barbs prevent backward slippage of the thread
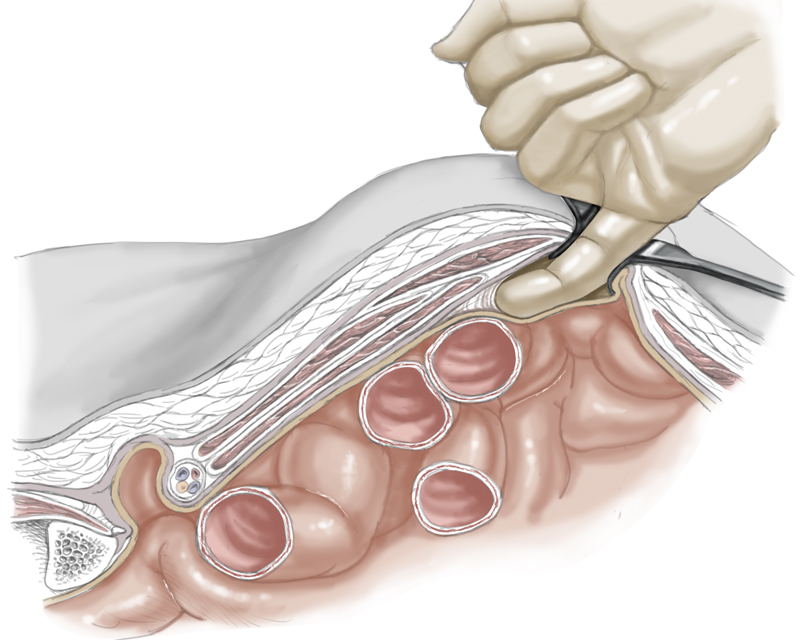
Variant - Incarcerated Hernia
- Here you see an incarcerated inguinal hernia
- A small bowel loop is trapped in the hernial orifice and cannot be spontaneously reduced
- After free dissection, a livid segment of the small bowel is visible
- If the bowel does not spontaneous recover, a small bowel segment resection in indicated since otherwise small bowel necrosis and perforation threatent
Femoral Hernia
Hernias that protrude through the vascular lacuna beneath the inguinal ligament are called femoral hernias. They occur preferentially in females, in whom they are the most common type of hernia. They are more difficult to diagnose inguinal hernias, among the differential diagnostic possibilities are enlarged lymph nodes.
Opening of the hernial sac revealed a small bowel necrosis, so an additional laparotomy was carried out in the lower abdomen, where a short segment of necrosis was also found; the incarceration had led to an ileus. Small bowel resection was performed.
OR-Video: Rives Technique Femoral Herniotomy
- Der Zugang erfolg analog zur Leistenherniotomie
- Auf der Haut eingezeichnet sehen sie gestrichelt die Projektion des Leistenbandes, unterhalbe des Leistenbandes die Schenkelhernie und als weitere anatomische Landmarken die Symphyse und die Spina iliaca anterior superior
- Subkutan verlaufende Venen werden ligiert
- Mit der monopolaren Diathermie wird bis auf die Externusapneurose präpariert
1 Access
- Access is gained as in inguinal herniotomy
- The dashed line on the skin marks the inguinal ligament, beneath the inguinal ligament lies the femoral hernia. Further anatomic landmarks are the symphysis and the anterior superior iliac spine
- Subcutaneous veins are ligated
- Dissection is performed with monopolar diathermy up to the external aponeurosis
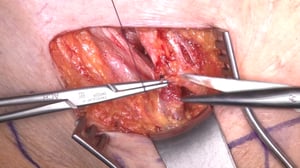
2 Opening of the Fascia transversalis
- The external aponeurosis is opened by incision of the intercrural fibers and the contents of the inguinal canal exposed
- Because this is a female patient, the inguinal canal contains the round ligament of the uterus
- After free dissection, the posterior wall of the inguinal canal is opened
- The femoral hernia is located under the transverse fascia, the vascular lacuna serves as the hernial orifice
3 Exposure of the Hernial Contents & Reduction
- The hernial contents, in this case the greater omentum, are removed from the vascular lacuna
- The hernial contents are repositioned intraperitoneally
- The hernial sac is closed
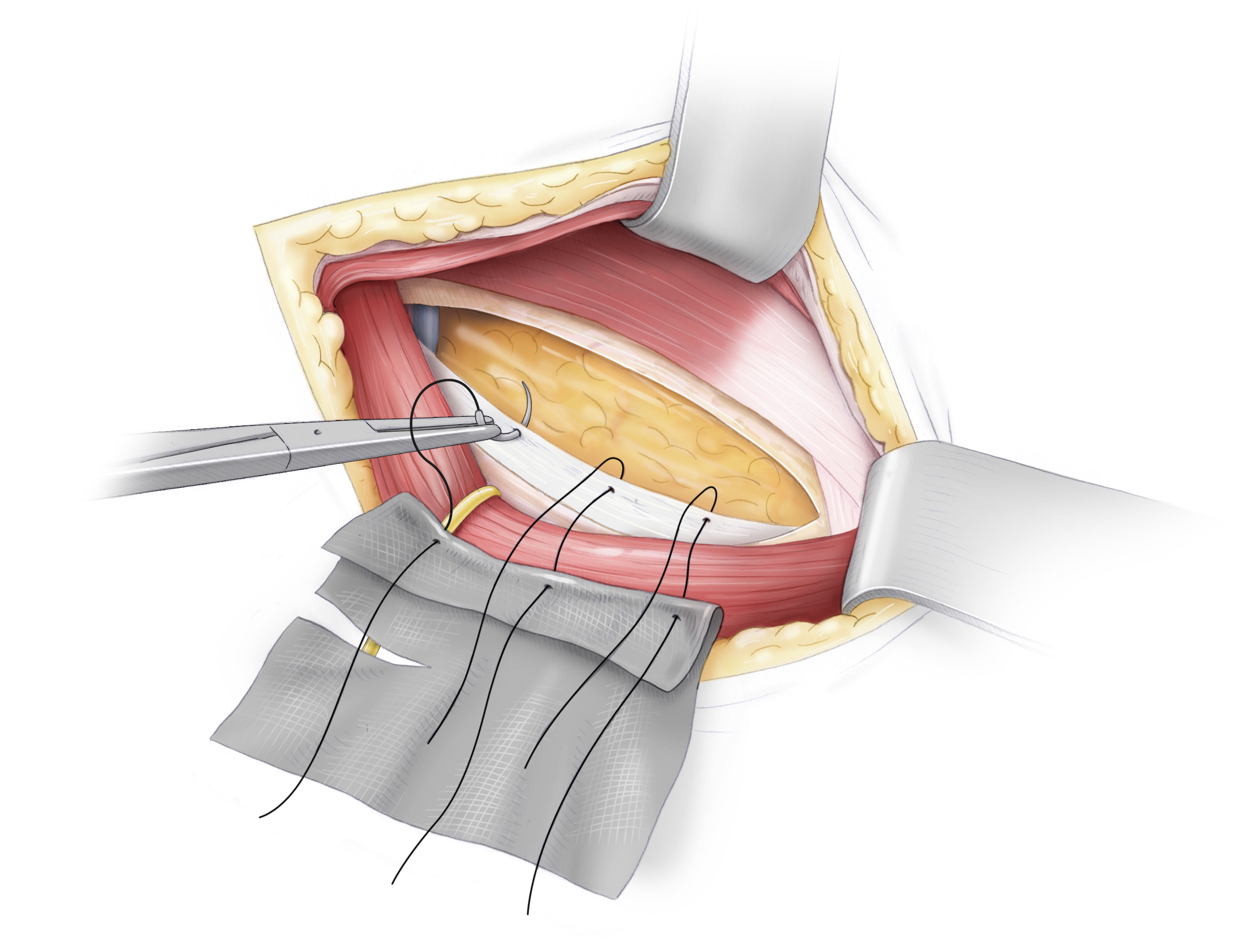
4 Preparation of the Mesh
- • A partially resorbable mesh is folded and attached at the crease to the pectineal ligament with nonresorbable suture
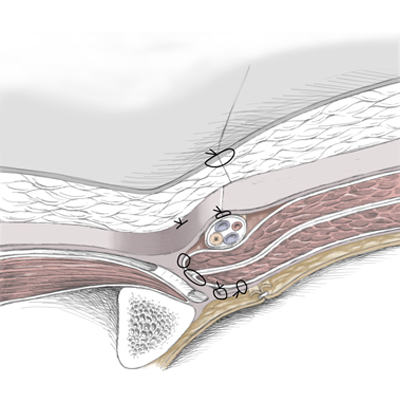
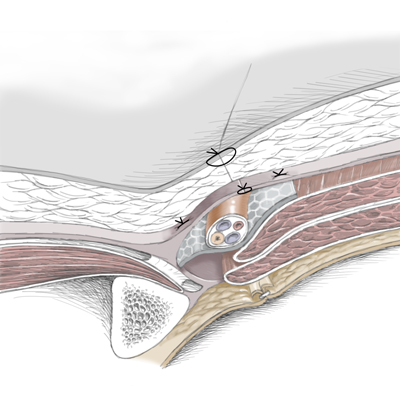
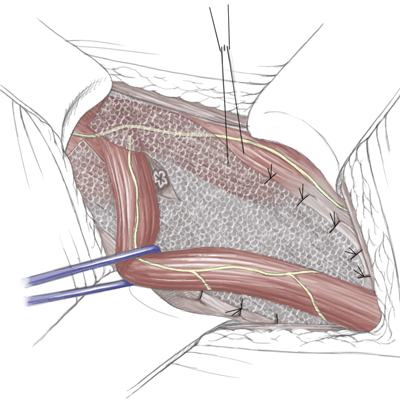
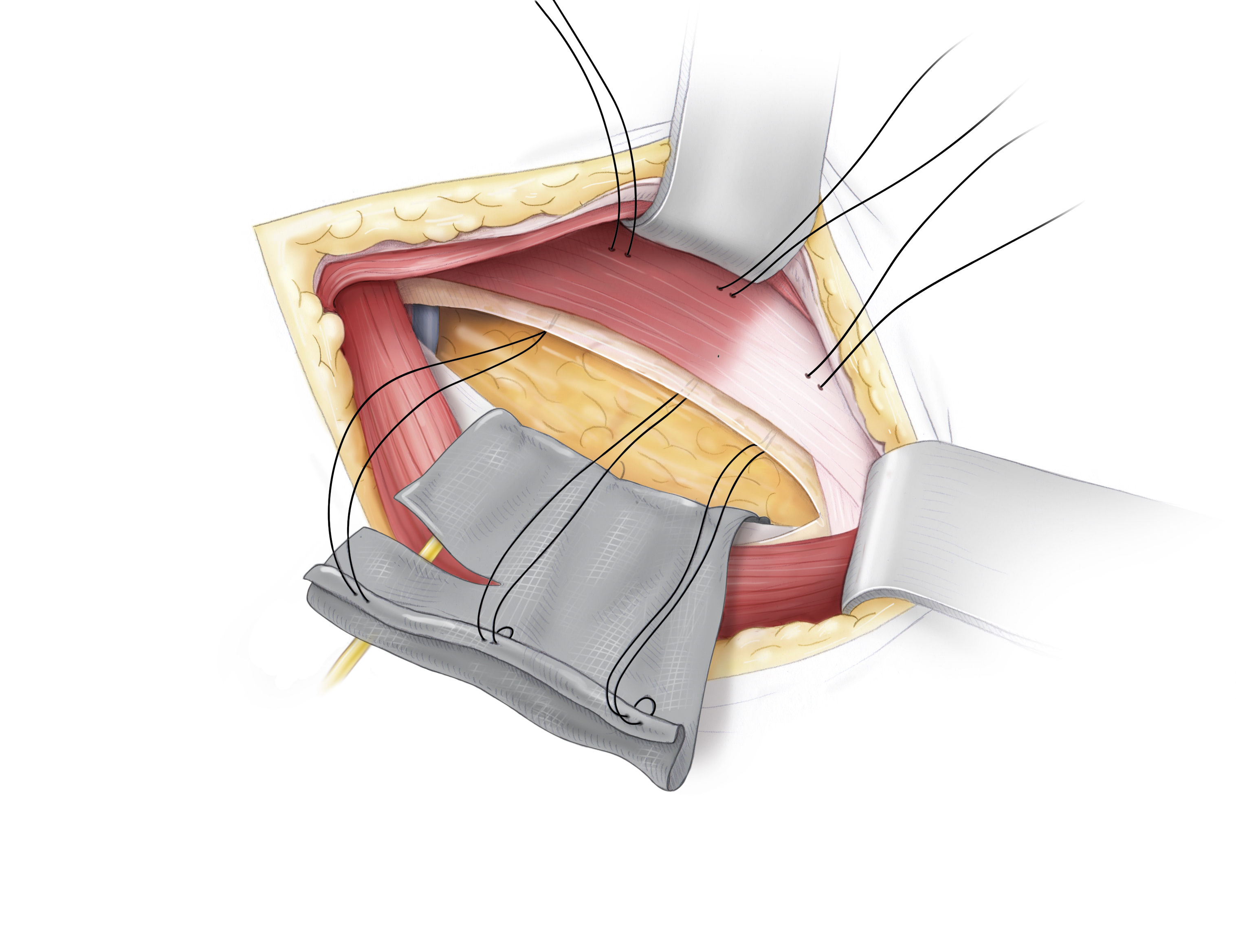
Schematic Drawing of OP
The folded mesh is affixed with prolene thread to the pectineal ligament. Attachment of the mesh By attaching the mesh with the vorgelegten (←?) threads, a caudal portion of the mesh is created which is folded retropubically The cranial portion is placed beneath the transverse fascia The hernial orifice and the hernial sac are thus covered by the mesh To allow passage of the inguinal canal structures, the mesh must be incised in a dovetail-like pattern (schwalbenschwanzartig) and, in this case, wrapped around the round ligament of uterus The mesh is finally affixed to the transversal fascia with PDS sutures
5 Fixierung des Netzes
- Mesh placement with the pre-placed sutures
- The mesh is additionally attached with nonresorbable sutures, which are stitched through the transversal fascia
OP Schematic Drawing
Mesh placement with the pre-placed sutures
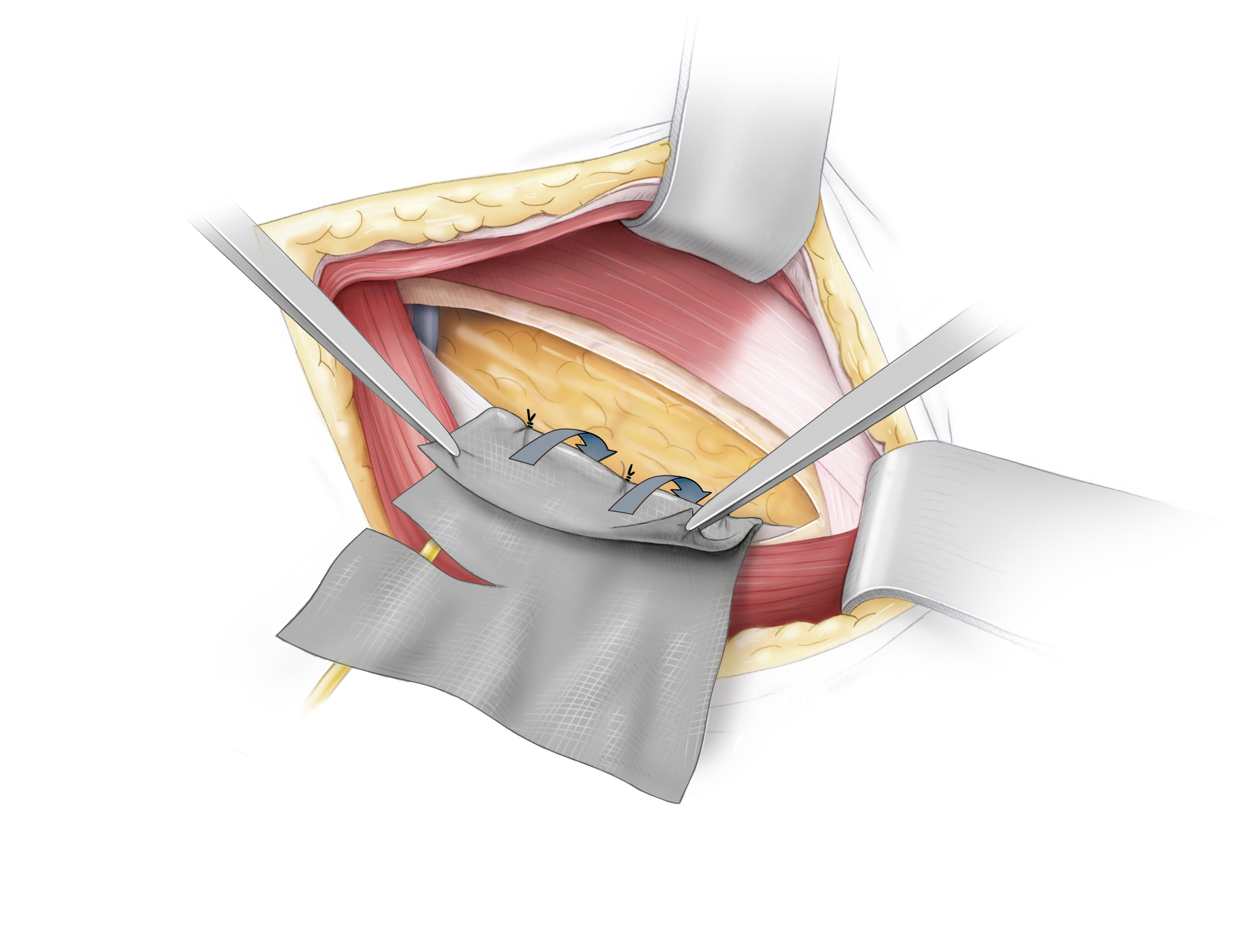
OP Schematic Drawing
The mesh is additionally attached with nonresorbable sutures, which are stitched through the transversal fascia
6 Closure of the Fascia transversalis
- After the mesh is placed and affixed, the groin is reconstructed
- To do this the transversal fascia is closed with several nonresorbable sutures
- Care must be taken to make the opening sufficiently large to accommodate the inguinal canal structures
7 Closure of the External Aponeurosis
- IAs in the Liechtenstein operation, the inguinal canal is now reconstructed
- The external aponeurosis is closed with simple interrupted stitches using nonresorbable sutures
- The superficial inguinal ring is thereby reconstructed
- Here too care must be taken that the opening is large enough to accommodate the structures of the inguinal canal
8 Drainage and Skin Closure
- The Redon drain is placed epifascially
- Subcutaneous suture follows with resorbable suture
- The procedure concludes with a resorbable intracutaneous suture and sterile adhesive bandage
Incisional hernia
Every abdominal wall incision, every abdominal operation leaves behind a
weak point in the integrity of the abdominal wall which, in further course, can lead to incisional hernia. In smaller hernias especially there is a risk of strangulation or incarceration. Through large hernial gaps entire organ clusters and the entire small bowel can herniate. Such hernias are difficult to repair. At one time, direct suture of the hernial gap was favored, especially for smaller hernias, today mesh repair of incisional hernias is standard.
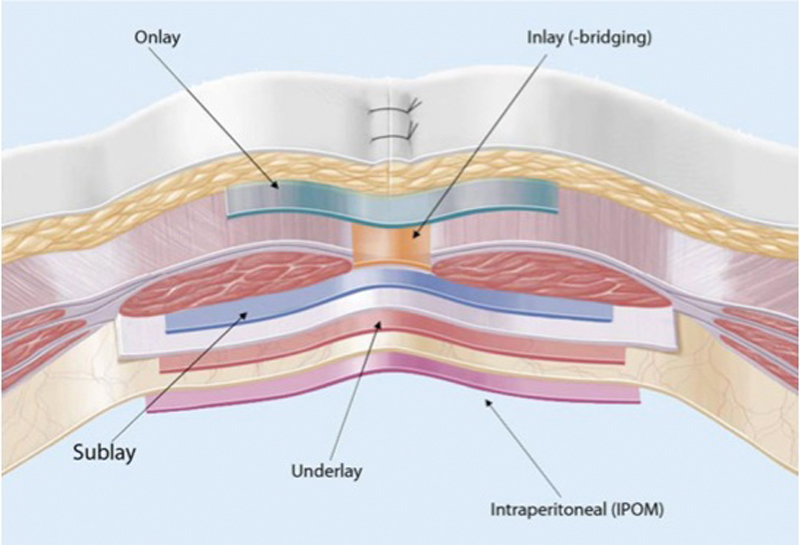
Positioning of the mesh can vary. In addition to open access, minimally-invasive herniotomy and mesh emplacement are appropriate in some cases.
Placement of the mesh on the rectus abdominis muscle from ventral is termed onlay technique, placement between the rectus bulges inlay technique.
In the inlay position, the mesh is placed retro-rectus but anterior to the posterior lamina of the rectus sheath. The inlay technique offers the best stability and lowest risk of recurrence. Dorsal to the posterior rectus sheath but anterior to peritoneum is the underlay position.
And finally, meshes placed intra-abdominally, i.e. beneath the peritoneum, are situated in the intraperitoneal onlay mesh (IPOM) position. These can be placed using either an open or laparoscopic procedure.
Wird das Netz von ventral auf die Rektusmuskulatur aufgebracht, spricht man vom Onlay-Verfahren.
Zwischen den Rektusbäuchen platziert, vom Inlay-Verfahren.
Hinter der Rektusmuskulatur aber vor dem hinteren Blatt der Rektusscheide liegt das Netz in Sublay-Position.
Dieses Verfahren bietet die beste Stabilität und das geringste Rezidiv-Risiko. Dorsal der hinteren Rektusscheide aber vor dem Peritoneum ist die Underlay-Position.
Netze schließlich, die intraabdominell, also hinter das Peritoneum gelegt werden, liegen in IPOM-Position. Diese können sowohl offen als auch laparoskopisch platziert werden.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma