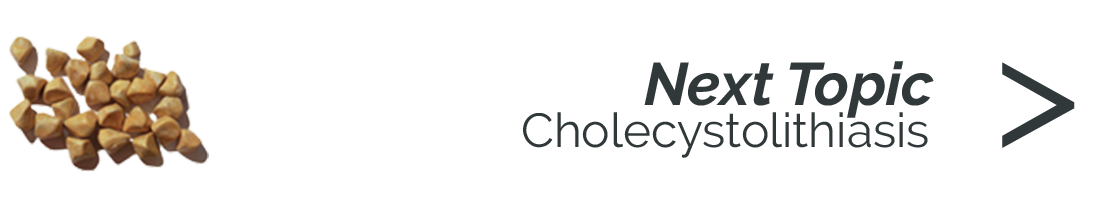
Anatomy
The liver is divided into 8 independent segments for surgical purposes, as first described by Couinaud.
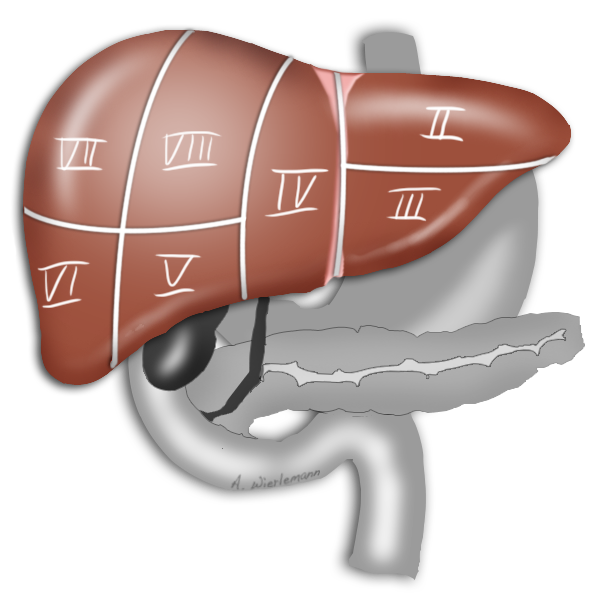
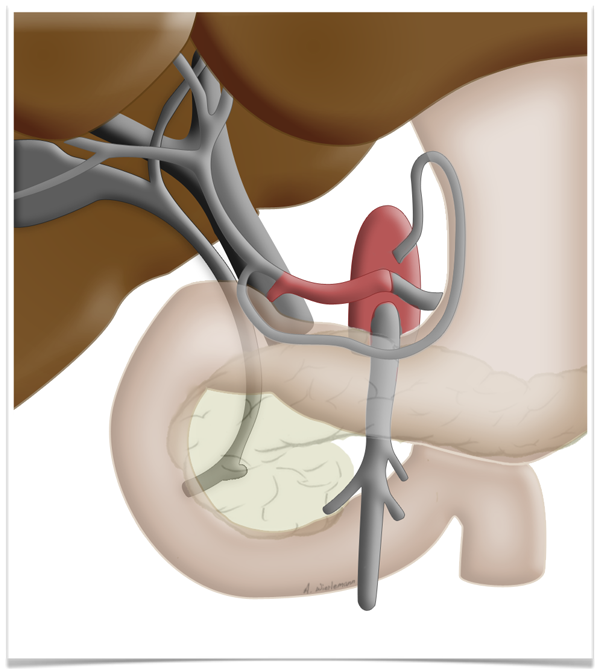
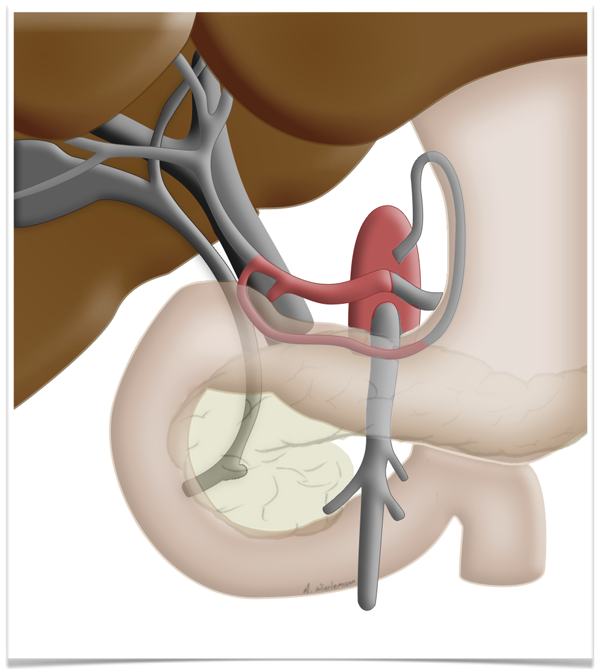
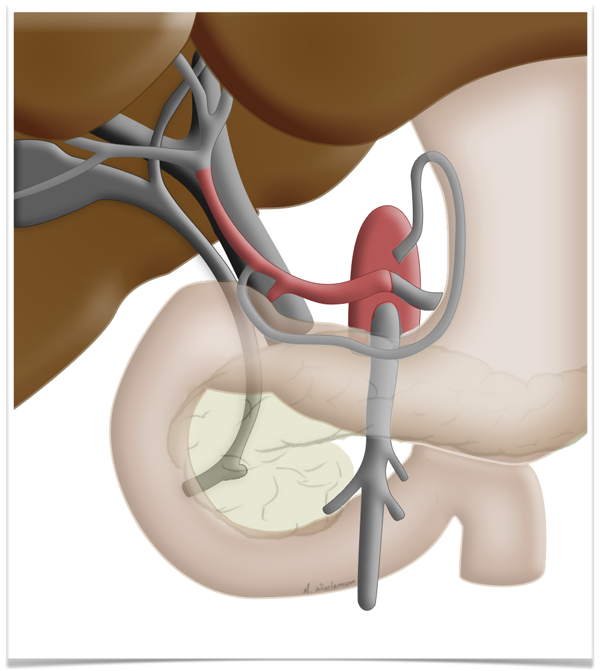
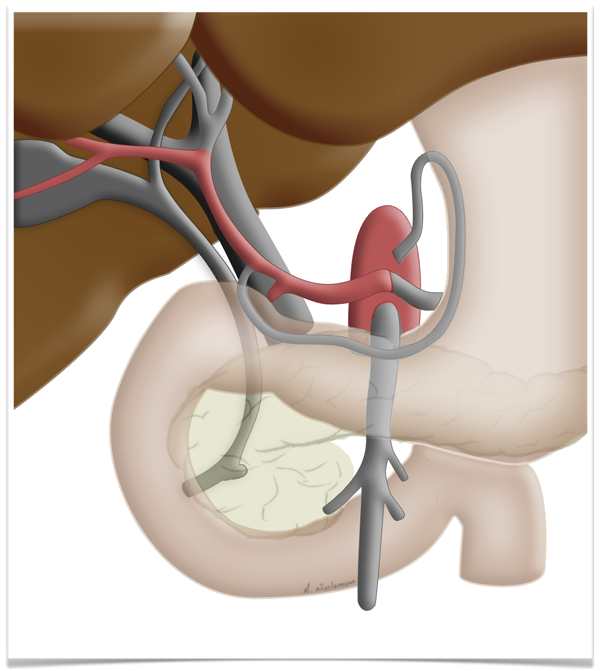
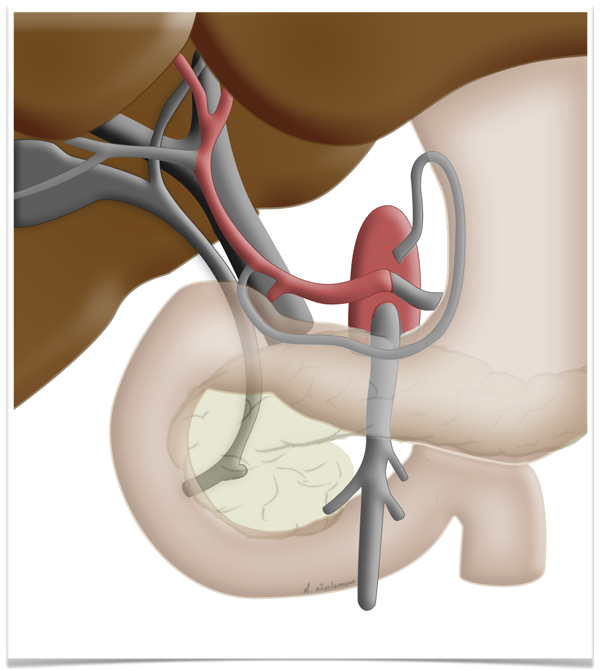
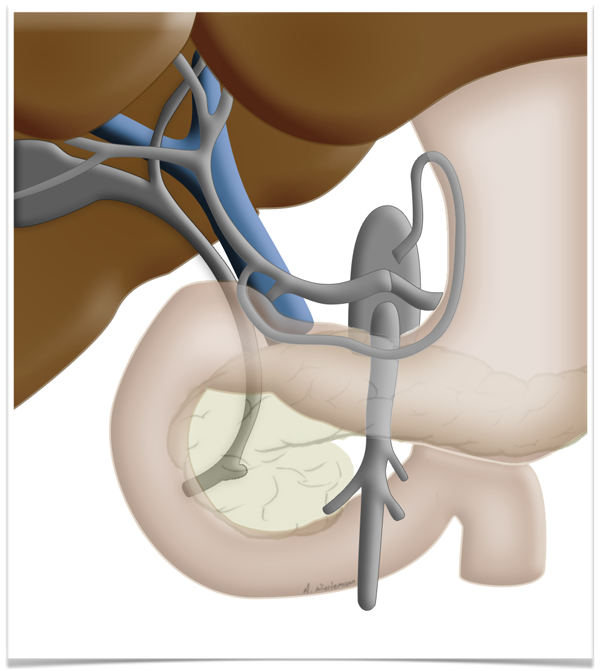
Arterial blood is supplied by the hepatic artery proper, which arises from the common hepatic artery. This in turn arises from the celiac artery, the first branch of the abdominal aorta beneath the diaphragm.
The hepatic artery proper divides into a left and a right hepatic artery. These, however, provide only 20% of the oxygen supply to the liver.
The remainder is provided by the portal vein, formed by the confluence of the superior mesenteric vein and the splenic vein, into which flows blood from the inferior mesenteric vein.
Liver Perfusion
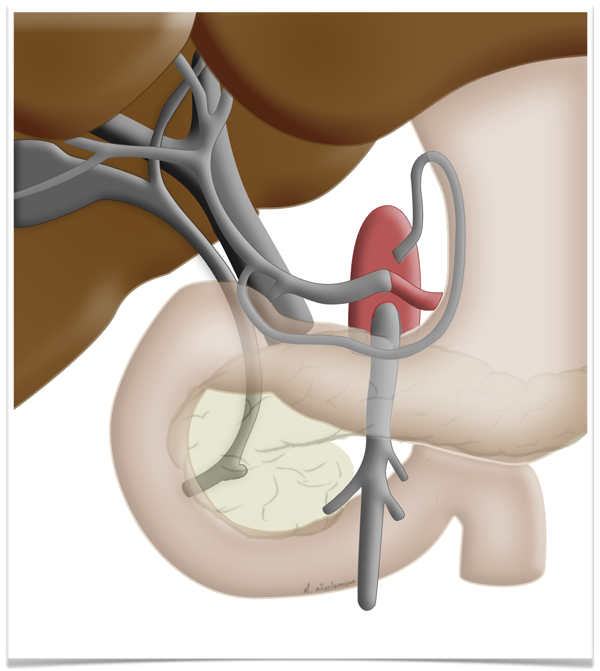
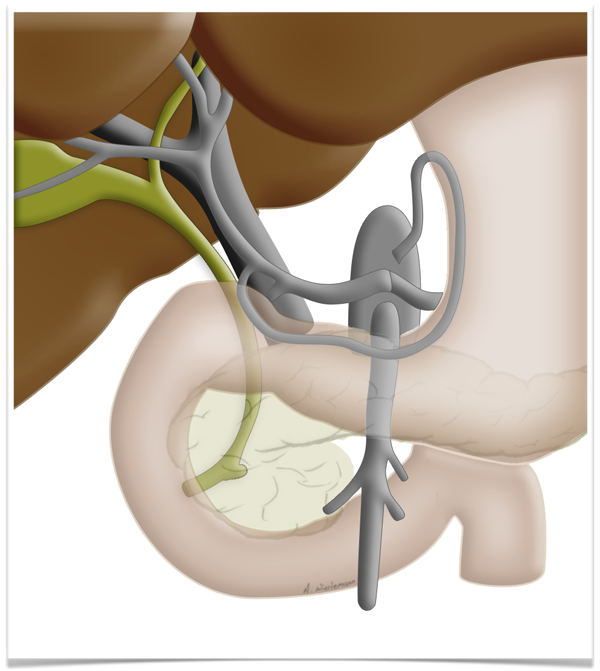
This peculiarity of the liver is exploited in so-called two-stage liver resection. If the tumor is so large that too little functional tissue would be left after resection, e.g. after an extended right hemihepatectomy, one can in a first step ligate the portal vein on the side
to be resected can be ligated in a first step. This deprives this part of the liver of most but not all of its oxygen supply, which produces a marked hypertrophy of the liver remnant, so that the resection can later be carried out without risking liver failure.
Regeneration Capacity
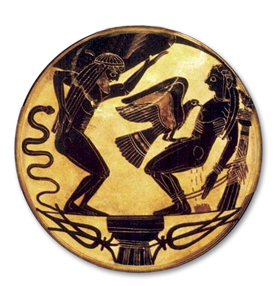
The liver’s remarkable capacity for regeneration after resection must have been known to the ancient Greeks. In Greek mythology, Prometheus stole fire from the Gods and is punished by being chained to a rock, where his liver is eaten by an eagle by day, and regenerates by night.
Basic Diagnostics
Diagnostic workup for the liver includes the patient’s medical history and clinical exam, specific laboratory parameters, plus CT, MRI, and endoscopic retrograde cholangiography (ERC).
In clinical exam, the liver is checked to determine whether it is palpable under the rib cage, is enlarged and painful when pressed. Murphy‘s sign, i.e. the patient wincing with a catch in breath while inhaling during palpation under the right rib cage, suggests an acute cholecystitis, Courvoisier's sign, painless jaundice and an enlarged gallbladder, may indicate pancreatic carcinoma.
Ikterus
Jaundice is a yellowish discoloration of the skin or sclera due to high bilirubin levels in the blood. A bilirubinemia above ca. 2mg/dl is visible clinically as jaundice of the sclera, later also of the skin. Jaundice can be accompanied by sometimes painful itching. The absence of coloration of the stool by biliverdin produces so-called acholic stools, which appear pale or even whitish.
As the bilirubin accumulates in the blood, it is increasingly excreted through the kidneys, giving the urine a dark, amber-beer color.

Pre-, Intra- and Post-Hepatic Jaundice
There are both obstructive and non-obstructive causes of jaundice. Jaundice can be caused pre-hepatically, e.g. by an increased accumulation of hemoglobin due to hemolysis. An intra-hepatic jaundice can arise from a conjugation disorder, i.e. the inability of the liver to transform indirect bilirubin into direct bilirubin which is excreted with the bile. Example include Gilbert's syndrome or cirrhosis of the liver. A post-hepatic jaundice may be caused by a mechanical obstacle that impedes drainage of the bile, i.e. a post-hepatic cholestasis. Possible causes include bile duct stones and tumors of the bile ducts or head of the pancreas.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma