Acute & Chronic Pancreatitis
Inflammations of the pancreas can be acute or chronic. The episodic course of chronic pancreatitis features histological changes to the pancreas, whereas acute pancreatitis can be followed by complete recovery of the pancreas. This applies of course only to the milder forms of acute pancreatitis.
The acute form can be divided into a relatively mild coursing edematous pancreatitis and a generally more severe coursing necrotizing pancreatitis.
Etiology
Among the possible causes of pancreatitis are gallstones, which can block the bile duct and thus back up the exocrine digestive enzymes, and excessive alcohol consumption. In ca. 20% of cases the etiology cannot be determined, these cases are termed idiopathic pancreatitis.
Clinical Picture & Diagnosis
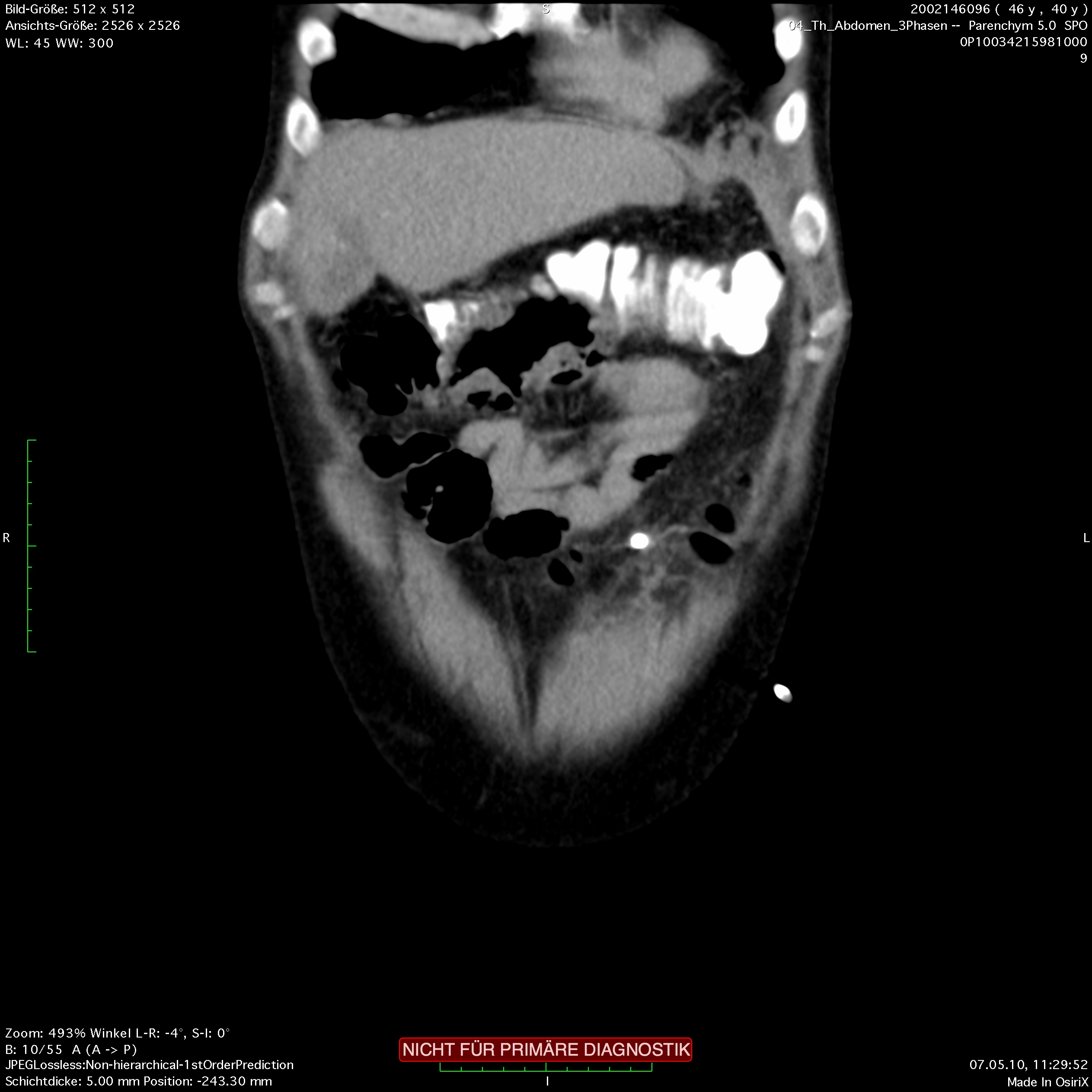
The clinical picture is marked by a dull pain in the upper abdomen which typically radiates to the back. At the flanks, periumbilical hemorrhaging can occur. This so-called Grey-Turner’s sign, or Cullen‘s sign, indicates a severe advanced pancreatitis and is prognostically unfavorable. In the laboratory diagnostics, the pancreatic enzymes are elevated. Special attention should be paid to the cholestasis values to recognize a possible biliary cause. Later in course, CT of the abdomen can reveal the extent of the necrosis, in early course this diagnostic tool has little value.
The acinus cells in the pancreas produce large volumes of digestive enzymes, so-called zymogens. To prevent these enzymes from digesting the tissues of the pancreas, they are transported in a bicarbonate-rich secretion to the duodenum, where they are activated. Premature activation within the pancreas can injure or even
destroy the organ. Increasing degeneration of the pancreas degrades its endocrine function, patients can develop an insulin-requiring diabetes mellitus. Digestion of the pancreas leads to typical chalk stains as a sign of the saponification of fat tissue. Neighboring organs, such as the transverse colon or stomach, can be eroded, resulting in fistulas and abscesses.
In the maximum picture of acute pancreatitis, superinfection of the necrotic foci can occur. This is associated with a severe disease course and sepsis as well as possible multiple organ failure. The severity of the disease at the outset and its potential mortality can be assessed applying Ranson's criteria for pancreatitis mortality, which are assessed at admission and at 48 h. The clinical relevance of this score is disputed since treatment is oriented on clinical course and not Ranson’s criteria.
Therapy
Treatment of acute pancreatitis consists primarily of eliminating the injurious agents if this is possible.
In a biliary pancreatitis, this mean removing the bile duct stones by ERCP. Strict abstinence from alcohol should be observed, not only if there is an ethyltoxic genesis. Otherwise therapy consists of fluid substitution, sufficient administration of analgesics, and monitoring in an intensive care unit.
Antibiotic therapy should not be given prophylactically, but only upon signs of infection or incipient sepsis.
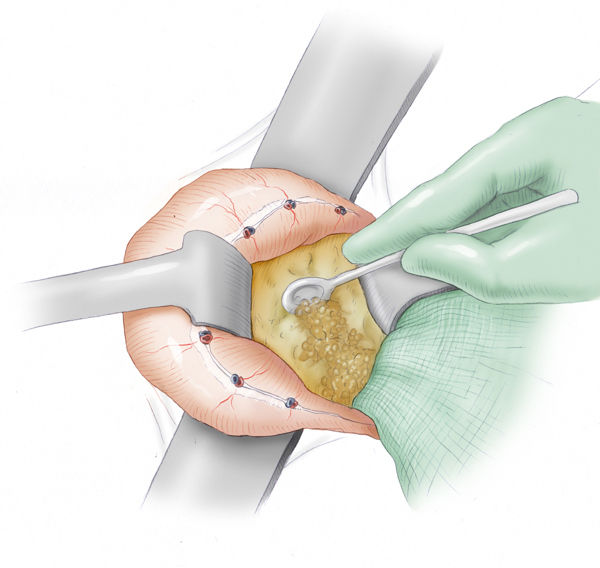
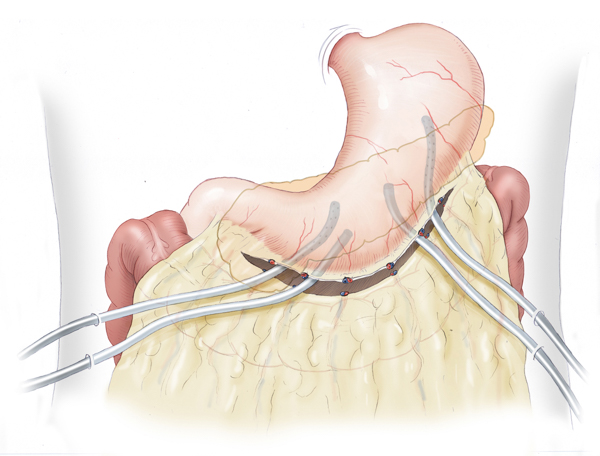
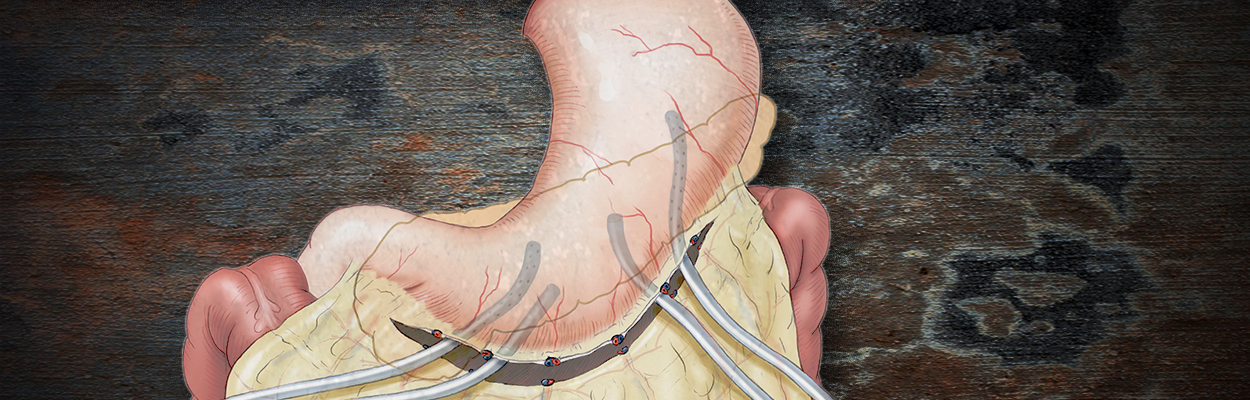
The decision for surgery in acute pancreatitis is made very cautiously. In its initial stage, the risk of bleeding is very high and patients do not benefit from early necrosectomy. If the disease follows a septic course, however, the superinfected necrotic foci can be removed surgically and a drainage system installed in the bursa omentalis. This generally consists of multiple inflow and outflow drains that are inserted from both sides into the bursa. Continuous lavage is used to dilute pathogens and remove necrotic material.
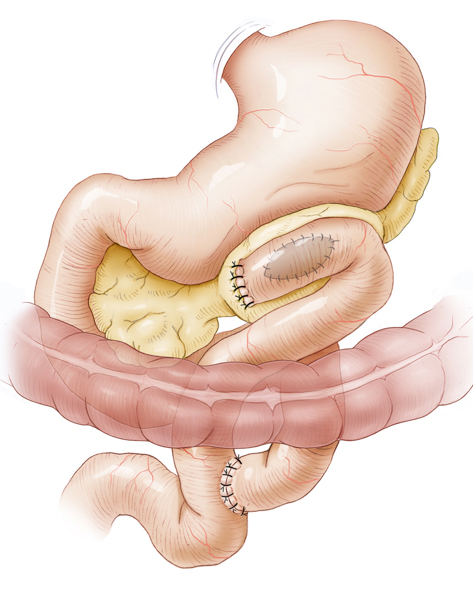
In chronic pancreatitis, partial or total obliteration of the pancreatic duct can occur. This obstructive form of pancreatitis involves a backup of bile with formation of pancreatic pseudocysts. Transgastral or percutaneous drainage can be used on these, but they will then usually recur. It is better to achieve permanent drainage by deroofing the cyst surgically and suturing a small intestinal loop to the cyst as a cystojejunostomy.
If chronic pancreatitis results in obstruction in the pancreatic head area, drainage surgery can be performed that resects the pancreatic head while preserving the duodenum. A small intestinal loop is then anastomosed to the free end of the pancreatic duct.



 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma