Classification
Perforations of the esophagus can be differentiated from ruptures, which are much less common. Perforations can be caused by instruments e.g. by a stomach probe or endoscope, or by ingested foreign objects such as a food bolus, animal or fish bones, even toys or dentures.
Spontaneous rupture of the esophagus is called „Boerhaave syndrome“ after its first describer, although the term emetogenic rupture is more appropriate since ruptures do not occur without a cause. Boerhaave syndrome ruptures can also occur without underlying prior injury to the esophagus following a episode with self-induced vomiting.
Classification
Instrumental
- Endoscopy
- Stomach probe
Penetration by foreign objects
- Food bolus
- Animal bone, fish bones
- Toys
- Dentures
Rupture (Boerhaave syndrome)
- Spontaneous, emetogenic tearing of the esophagus after self-induced vomiting
Medical History & Clinical Findings
Rupture of the esophagus is accompanied by extreme retrosternal pain, patients report „annihilating pain“ localized in the thorax or the epigastrium. Because mediastinitis or pleural empyema can quickly develop, patients may exhibit symptoms of shock after only a brief time. Also relevant to prognosis is the lesion’s etiology.
Diagnosis
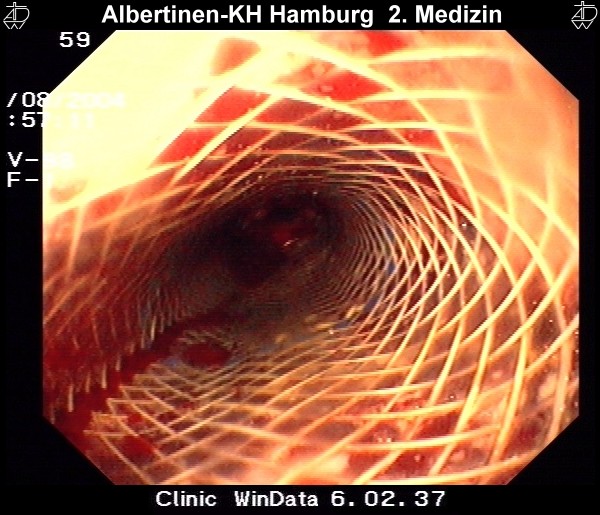
Fluoroscopy with a water soluble contrast medium is best suited for depicting the perforation or rupture, esophagogastroscopy can confirm the finding morphologically.
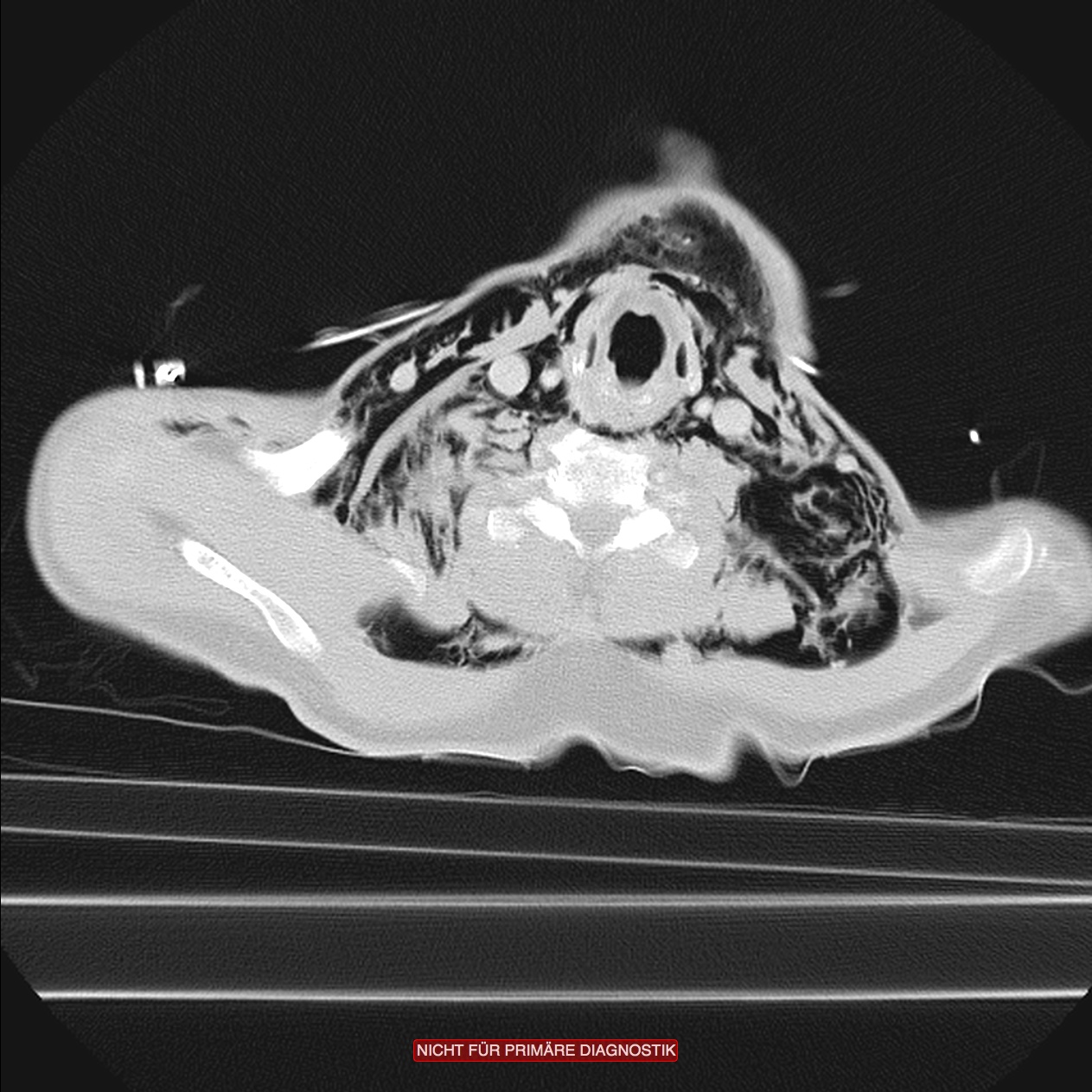
CT can detect a mediastinal emphysema or pleural empyema. The principal always applies: „Diagnosis should never delay the start of therapy!“
Therapy:
Iatrogenic lesions caused, for example, by a stomach probe have a better prognosis if strict fasting is immediately started and the patient treated with antibiotics. Much more important however is the temporal course. The longer the interval between trauma and therapy, the poorer the prognosis. Untreated, all patients with an esophageal rupture or perforation die.
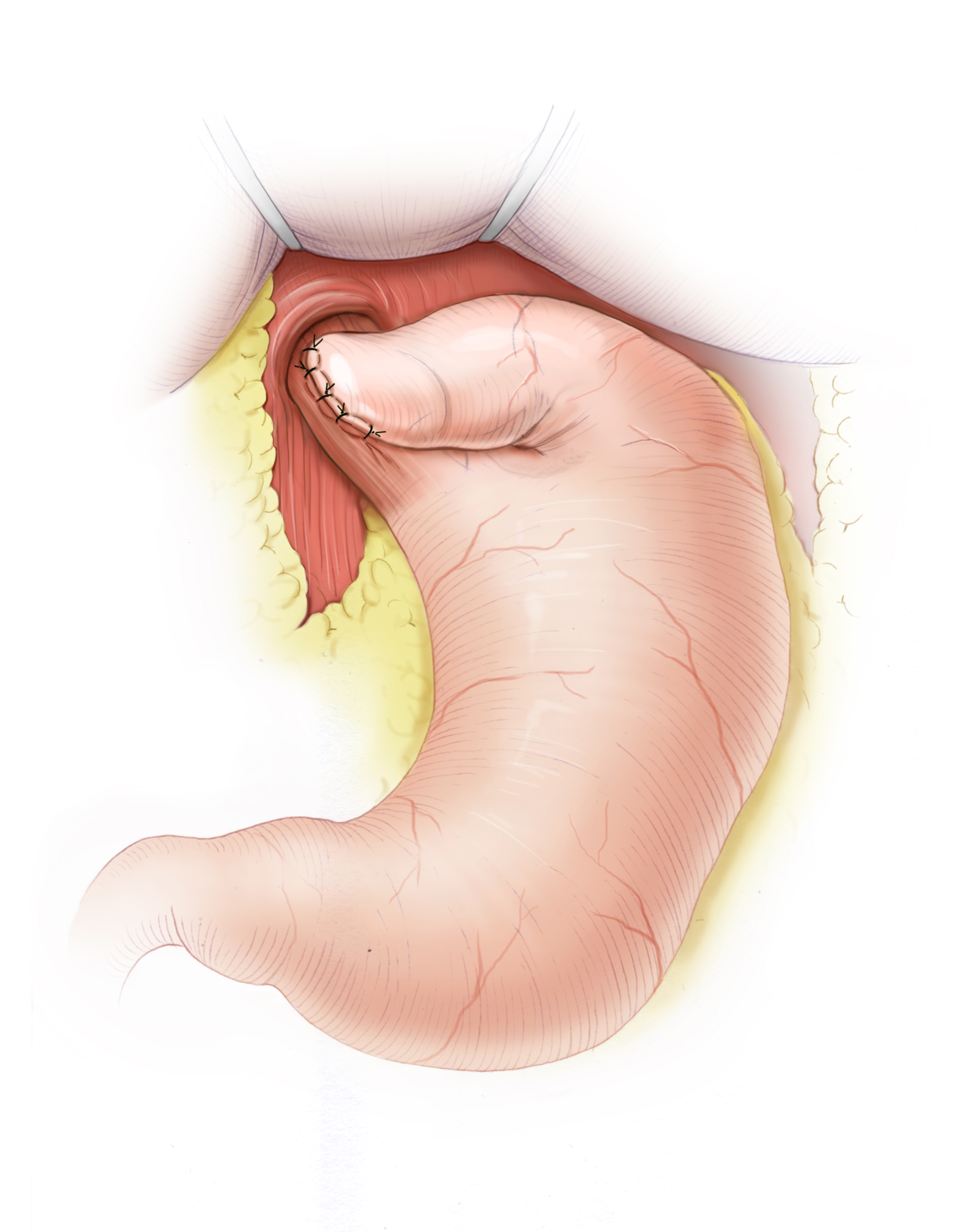
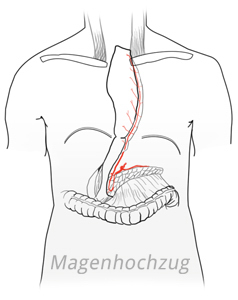
Smaller lesions can be covered with a stent. Distal defects are sutured over and closed with a fundoplication. Intrathoracic defects are repaired with a pleural flap. As ultima ratio remains esophageal resection and reconstruction using gastric pull-up or colon interposition. This is accomplished in a two-step procedure allowing the patient to stabilize in the interval and adequate treatment of a sepsis.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma