Introduction
Treatment of CIBD belongs to the broad domain of internal medicine. Surgical treatment is limited to dealing with the complications of CIBD. The main types of CIBD, ulcerative colitis and Crohn’s disease, have some features in common but also definite differences.
Symptoms
The two diseases have very similar symptoms. Both types of CIBD are characterized by abdominal pain as well as bloody and mucous diarrhea. Both may follow an intermittent or continuous course.
Diagnosis
Clinical suspicion of a CIBD can be confirmed by colonoscopy. In addition to characteristic macroscopic changes, biopsies can be taken to confirm the diagnosis histologically. For ulcerative colitis, stepwise biopsies are taken from the entire colon; this disease is almost never seen in the small bowel.
In Crohn’s disease, suspicious areas are targeted for biopsy. Since this disease can affect the entire gastrointestinal tract, a gastroscopy may also be necessary as well as dynamic MR enteroclysis (Sellink method) of the small intestine. Enteroclysis is a radiological procedure that can be done conventionally with x-ray or with magnetic resonance imaging (MRI).

Histology
Ulcerative colitis is limited to the mucosa and submucosa. Histologically, crypt abscesses may be seen, but no granuloma. Colitis is an intramural disease.
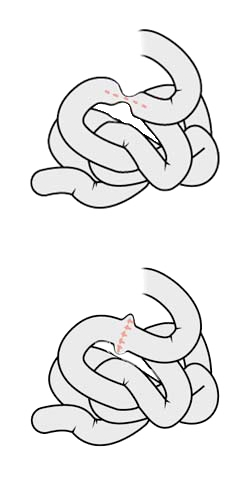
In Crohn’s disease, the definitive histologic finding is granulomas. These cannot, however, be demonstrated in every case. Crohn’s disease is a transmural disease that affects all wall layers and tends to formation of fistulas.
Clinical Symptoms
The clinical picture of ulcerative colitis usually involves, as the name suggests, a colitis. It always begins in the rectum and normally affects only the colon. Only rarely, in the context of a so-called "backwash ileitis", is the terminal Ileum also affected. The pattern of spread of ulcerative colitis is continuous.
In Crohn’s disease, the entire gastrointestinal tract may be affected. The disease follows an intermittent course. There is almost always inflammation of the terminal ileum, i.e. terminal ileitis. Clinically, Crohn’s disease presents with pain in the right lower abdomen and possibly a palpable conglomerate tumor. Fistulas may also be the first manifestation of Crohn’s disease, occurring as enterocutaneous, entero-enteral, or perianal fistulas. In addition, stenoses or strictures secondary to inflammatory changes may become symptomatic.
Complications
Ulcerative colitis is associated with a clearly elevated risk of colon carcinoma. Toxic megacolon is another possible complication, a life-threatening disorder characterized by massive dilatation of the colon.
Crohn’s disease may involve every known type of fistula, whether bowel-to-bowel fistula with formation of short bowel syndrome or enterovesical fistula with recurrent urinary tract infection. Fistulas of the skin, i.e. enterocutaneous fistulas, are also possible. These fistulas may be complicated by abscesses.
A fistula is defined as an unnatural connection between two hollow organs or between a hollow organ and the skin
Surgical Procedures
In surgery for Crohn’s disease, always as little should be resected as possible. The patient does not profit from radical surgical resection since a recurrence can occur anyway. It should always be attempted the resect as little of the small bowel as possible, since otherwise after repeated interventions a short bowel syndrome threatens.
If a stricture is present in the small bowel, it can be treated without resection by opening the bowel longitudinally and closing it again diagonally. This so-called stricturoplasty effectively treats the narrowing of the bowel without having to resect the small bowel.
In surgery on ulcerative colitis, the entire colon and rectum are removed, thus healing the patient of the disease. The intestinal continuity is reconstructed by an ileoanal anastomosis with formation of a J pouch, which performs as a reservoir. Stool frequency after this procedure is about 5 to 10 stools per day. This may appear to be a lot and incompatible with a good quality of life, but considering that patients with therapy-refractive ulcerative colitis pass stool up to 30 times a day, it does indeed represent a major improvement.
An ileal pouch-anal anastomosis is always preceded by a double-barreled ileostomy to ensure complication-free healing of the anastomosis.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma