Introduction
As late as the 1970s, surgery was often used to threat gastric and duodenal ulcers. Since the introduction of effective drugs for suppressing stomach acid and the discovery of H. pylori by the Australians Barry Marshall and John Robin Warren, the use of surgery has declined dramatically.
„No H.P. or damage from NSAIDs -- no ulcer"
– Günter J. Krejs, Graz, 2000Surgery today represents only a alternative treatment in cases refractive to drug therapy. For their discovery and description of the pathomechanisms by which H. pylori infection promotes the development of gastritis and ulcer, they were awarded the 2005 Nobel Prize in Medicine.
The postulate that has come to be known as Schwarz's dictum: „No acid – no ulcer “ (Karl Schwarz, 1910) retained its validity for decades. Today one would more likely say: „No H.P. or damage from NSAIDs – no ulcer“ (Günter J. Krejs, Graz, 2000)

Etiology
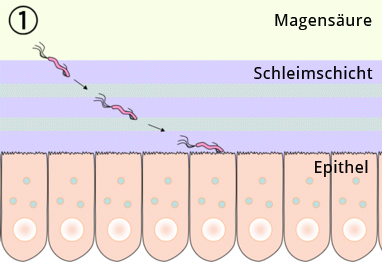
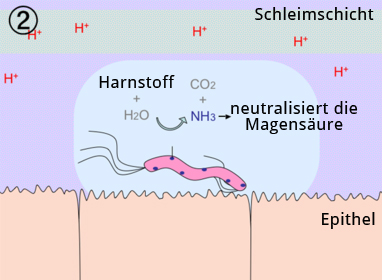
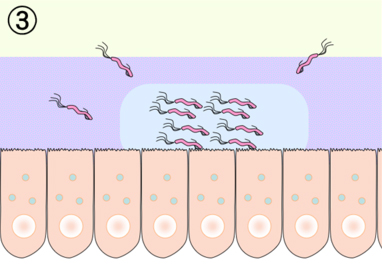
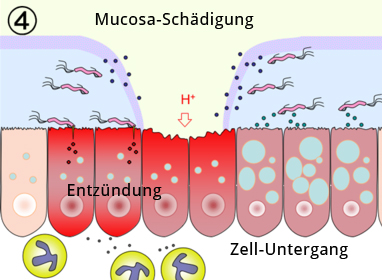
The main risk factor for development of an ulcer is infection with H. pylori. An ulcer, that is an erosion of the muscularis mucosae that can penetrate to the deep wall layers, arises from a imbalance of aggressive mucosal erosive and mucosal protective factors. The damaging effect of gastric acid and pepsins is countered by the so-called mucosal barrier, which is comprised of an insoluble mucus layer that overlies the epithelium of the stomach, and by the secretion of bicarbonate. Infection with H. pylori disturbs epithelial function and the barrier against the damaging effects of gastric acid breaks down. Patients infected with H. pylori have an up to 10-fold higher risk of developing an ulcer.
Development of an ulcer is a multifactorial event, as evidenced by the high H. pylori infection rate in the population: H. pylori infections affect 30% to 60% of the population, but only 2% develop ulcer disease.
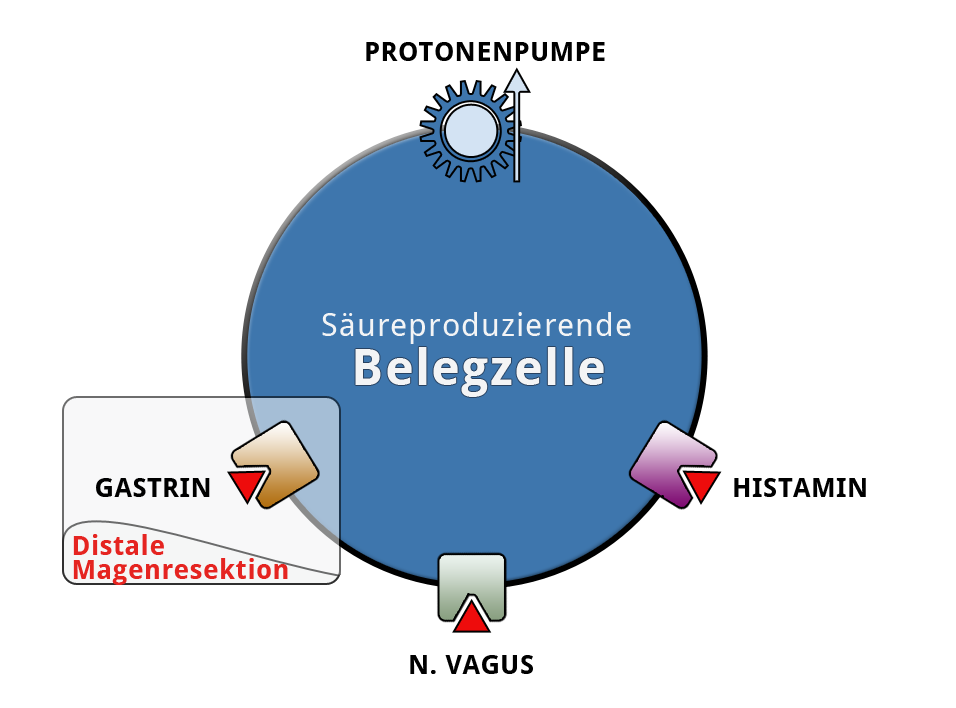
Acid production by the parietal cells in the stomach is regulated by gastrin, which is chiefly formed by G cells in the pyloric antrum. A proton pump in the parietal cells enriches the gastric contents with H+-ions and lowers the PH value. The parietal cells are stimulated by gastrin and directly by branches of the vagus nerve. Histamine can also stimulate the parietal cells to acid production.
Ventricular Ulcers
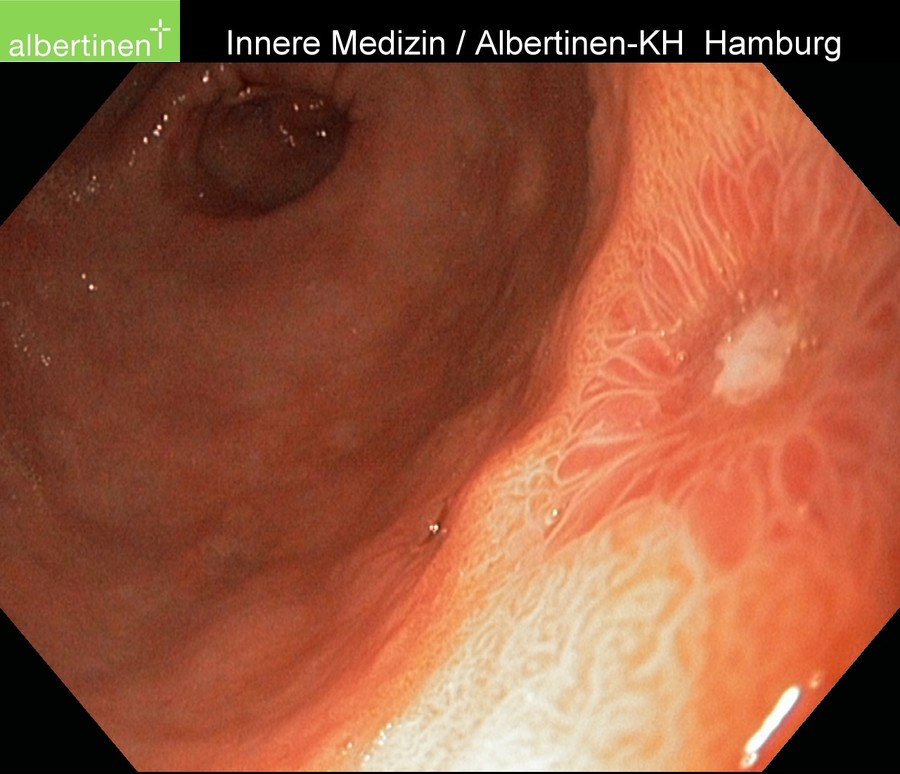
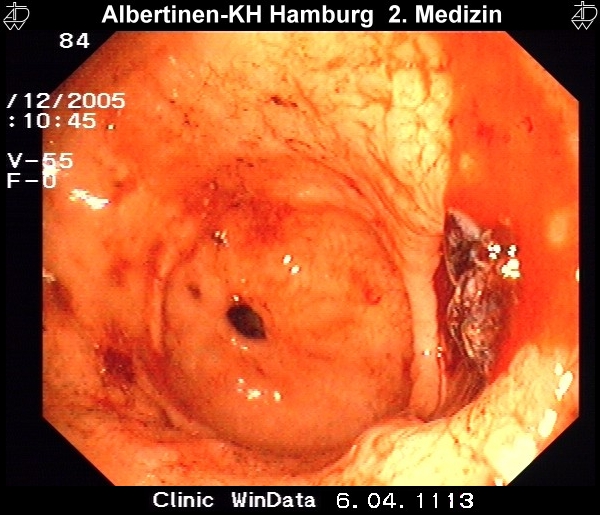
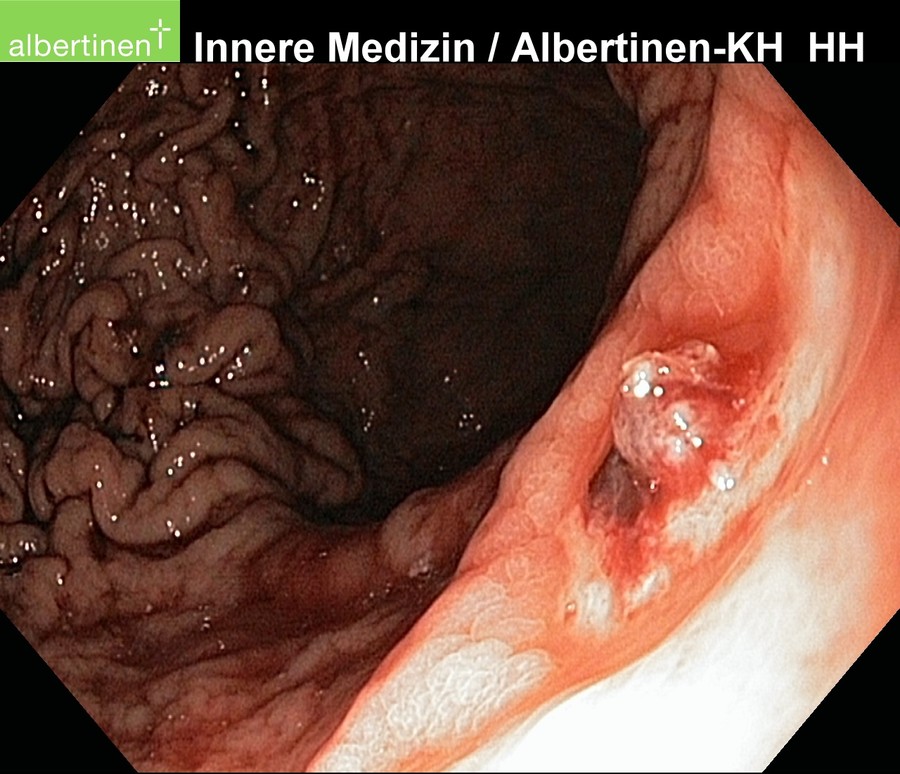
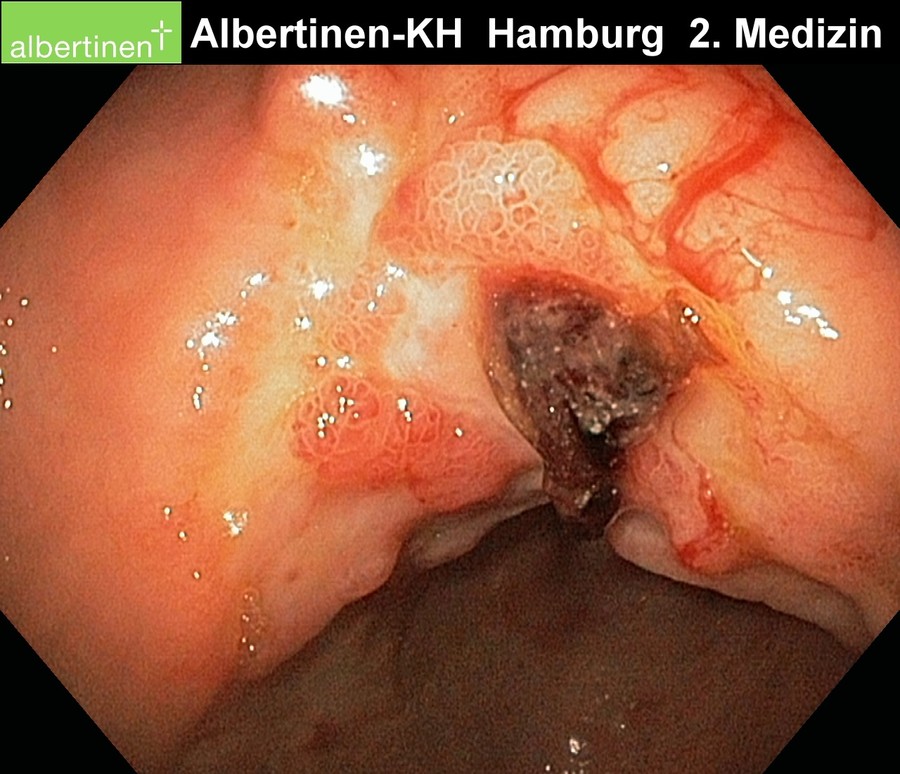
Stomach ulcers are typically located in the lesser curvature, at the transition of the body of the stomach to the antrum. In principle every stomach ulcer must be clarified histologically from biopsy of its floor and margin since gastric carcinoma is a possible cause of ulceration.
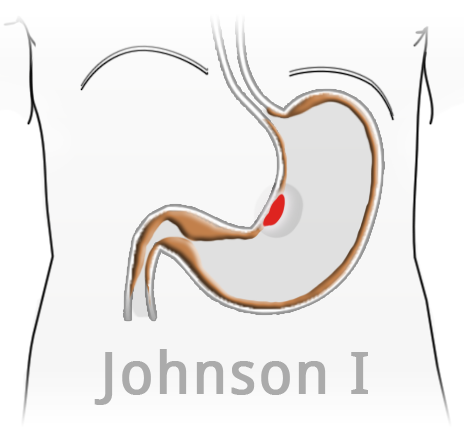
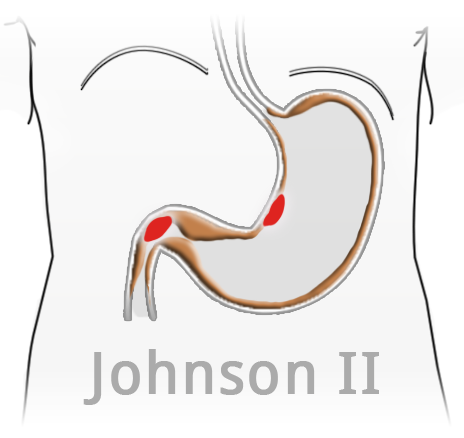
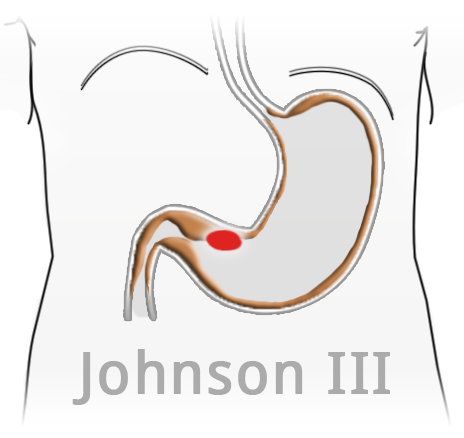
Ulcers with an atypical location are especially suspicious. Johnson distinguishes 3 different types of ulcer according to location, lesser curvature ulcers in loco typico (Johnson I), combined duodenal and ventricular ulcers (Johnson II), and prepyloric ulcers (Johnson III). Ulcers in the gastric fundus are extremely rare and suggest an change in the local mucosa to an antrum-like type.
Duodenal Ulcers
I
Duodenal ulcers are much more common than gastric ulcers. They are usually located in the duodenal bulb, i.e. in the area immediately distal to the pylorus. Ulcers located further distal in the duodenum can be a sign of a Zollinger-Ellison syndrome.
In Zollinger-Ellison syndrome a gastrin-producing tumor, typically located in the pancreas or duodenum, stimulates massive production of gastric acid. The resulting hyperacidity is combined with an atypically located duodenal ulcer. Diagnosis is made by standard procedures plus determination of serum gastrin levels.
Symptoms
Epigastric pain is a key symptom of ventricular ulcers and increases in classical cases following food intake. In duodenal ulcers, patients experience an lessening of symptoms postprandial. Reliable classification based on symptoms, however, is not possible due to their low specificity.
Diagnosis
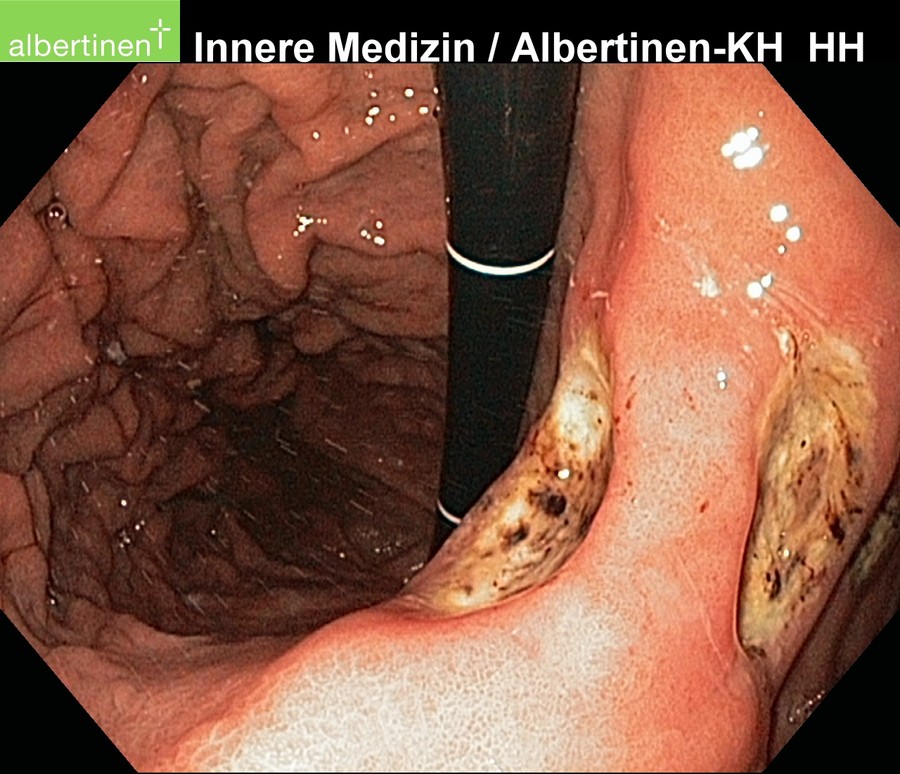
The diagnostic method of choice is endoscopy. It can not only reliably locate the ulcer, but also allows the taking of biopsies for histological evaluation and H. pylori diagnosis. In gastric ulcers several biopsies should always be taken both from the floor of the ulcer and its margins. This allows a representative finding as to whether it is benign or malignant (or premalignant). Duodenal ulcers are rarely malignant and in a high percentage of cases infected with H. pylori. Biopsies are usually only taken in very large, so-called giant duodenal ulcers.
Diagnosis of H. pylori can be made under the microscope, where it appears as acid-fast, rod-shaped bacteria, or clinically using the very quick and practical urea breath test. The latter is based on the ability of the bacterium to break down urea with the enzyme urease. An indicator dye binds to the urea and rapidly leads to a change in color if H. pylori urease is present. Thus in just an hour without great apparative expenditure the presence or absence of H. pylori infection can be established.

Therapy
Ventricular and duodenal ulcers are treated very differently. Common to both is that the treatment is primarily conservative. Proton pump inhibitors and H2 antagonists are effective drugs that lower gastric acid production by the parietal cells. Failure of conservative therapy or complications such as refractive ulcer bleeding or perforation are indications for surgery.
Eradication therapy for H. pylori infection consists of combination therapy with proton pump inhibitors and antibiotics. In the French triple therapy, pantozol is combined with amoxicillin and clarithromycin, in the Italian triple therapy metronidazole is used instead of amoxicillin. The latter therapy is carried out over a period of 7 days, after a few weeks the patient is reexamined. This does not need endoscopy, but can be done with a special breath test. The latter, however, does not allow assessment of macroscopic or histological changes, thus usually rendering follow-up gastroscopy unavoidable.
Therapy – Ventricular Ulcer
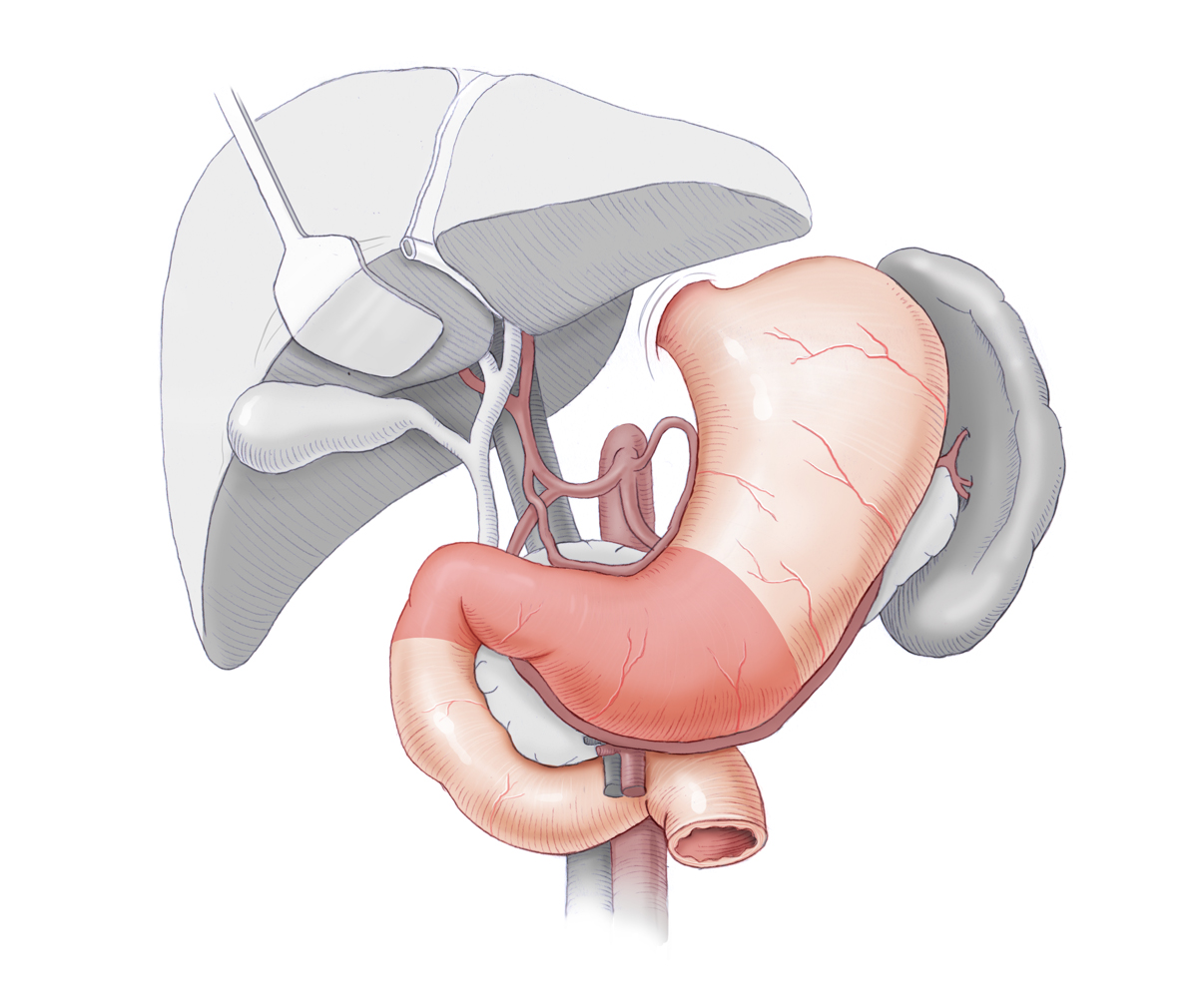
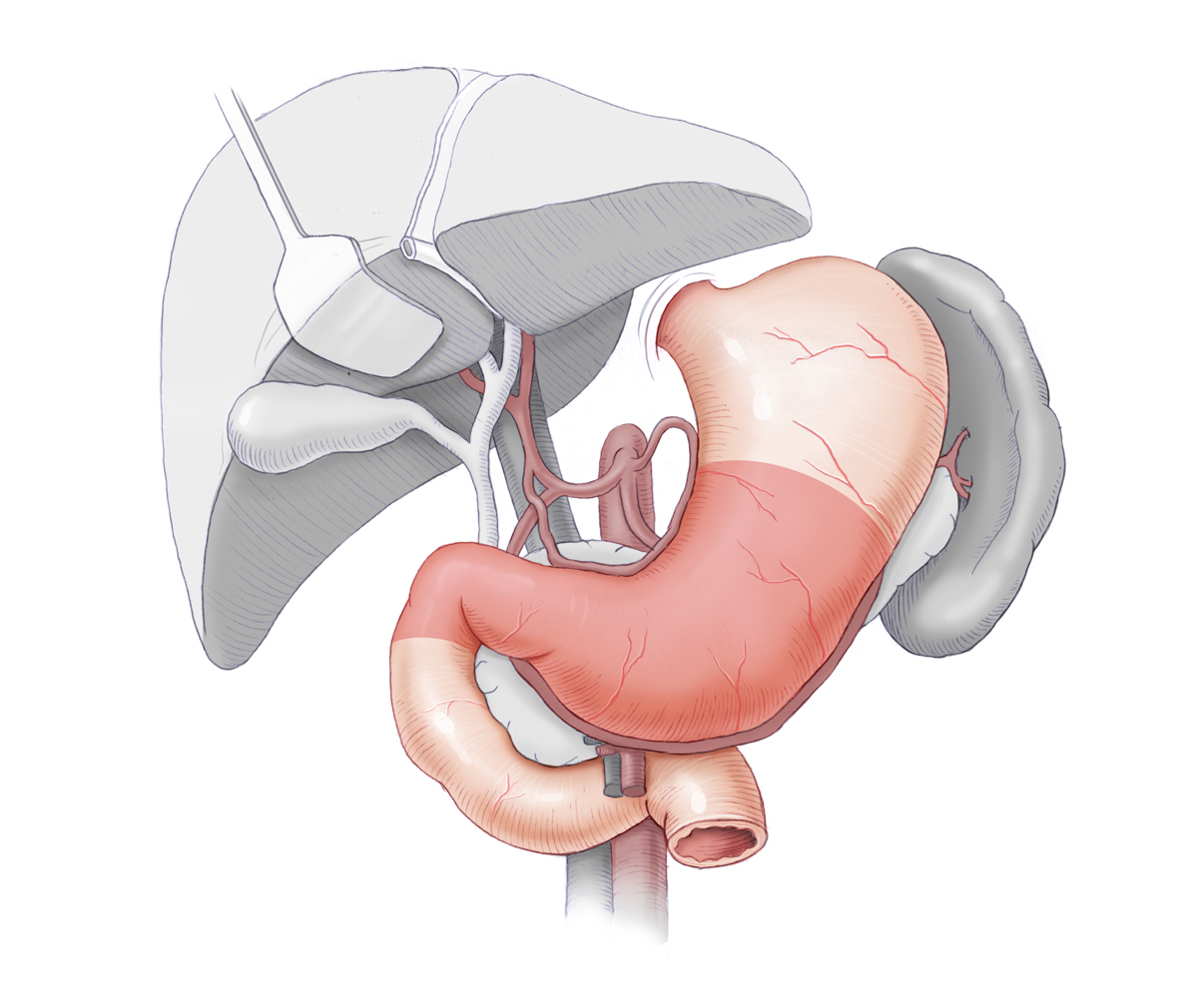
In gastric ulcers suspected malignancy can also be an indication for surgery. If despite inconspicuous histology, adequate acid blocking, and H. pylori eradication there is no trend toward healing, malignancy must be suspected. The goal of gastric ulcer surgery is therefore partial gastrectomy and histological clarification of the ulcer. Depending on its location, limited 1/3, 2/3, or subtotal resection are carried out. This removes not only the ulcer itself, but also markedly reduces acid production because the majority of parietal cells are resected with the antrum. Moreover, the remainder of the stomach is partially denervated, which diminishes the stimulating effect of the vagus nerve. In the antrum gastrin is also produced, so that this factor is also lessened.
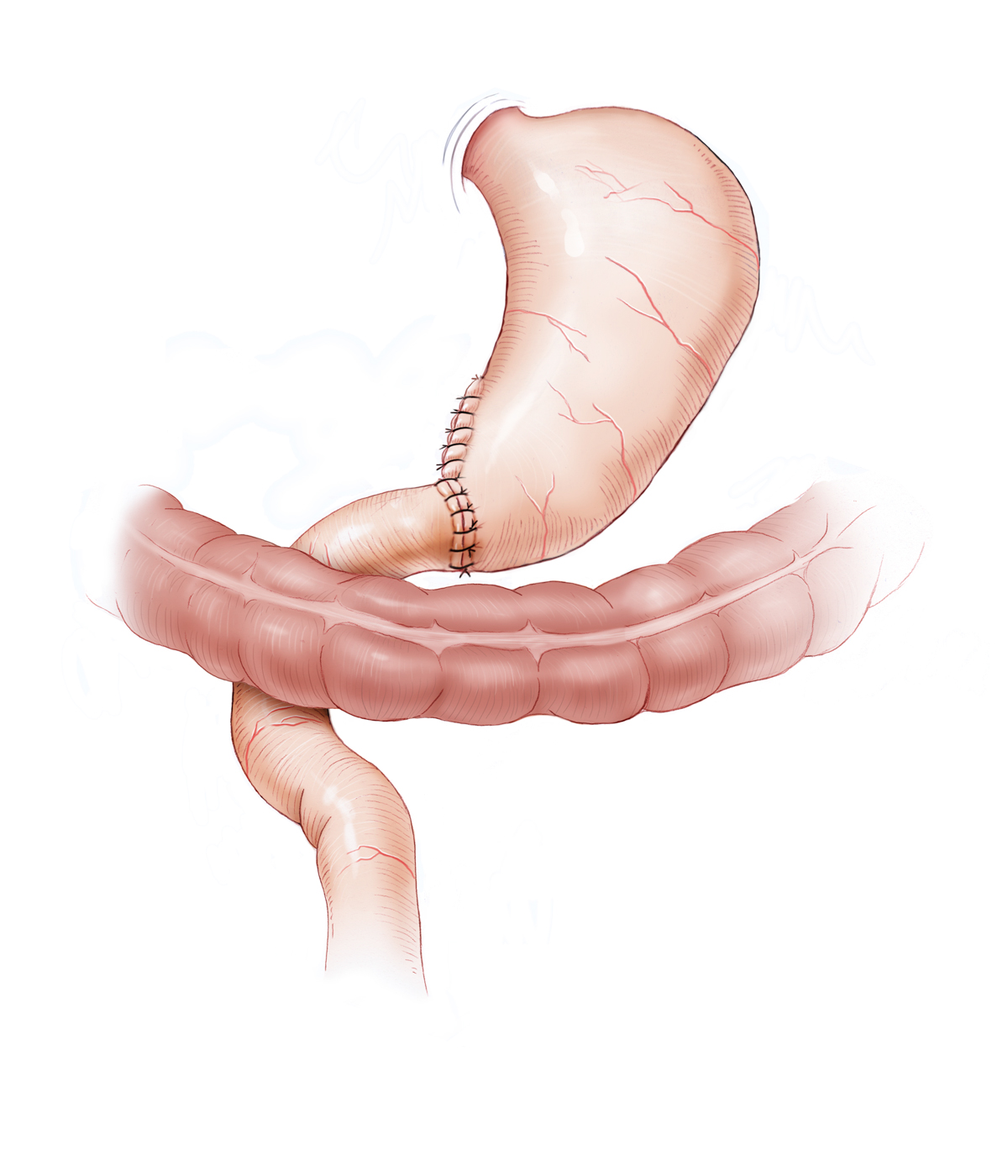
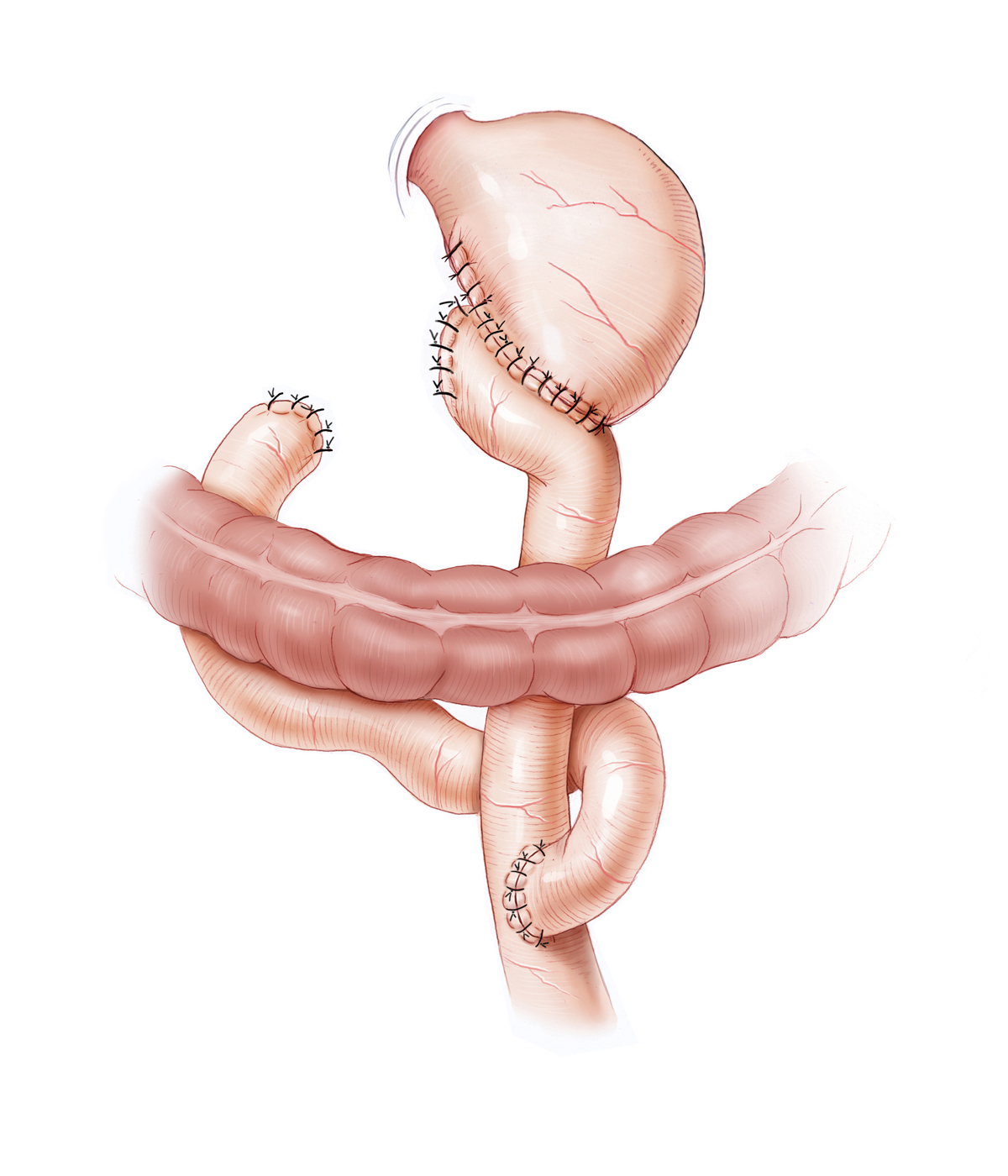
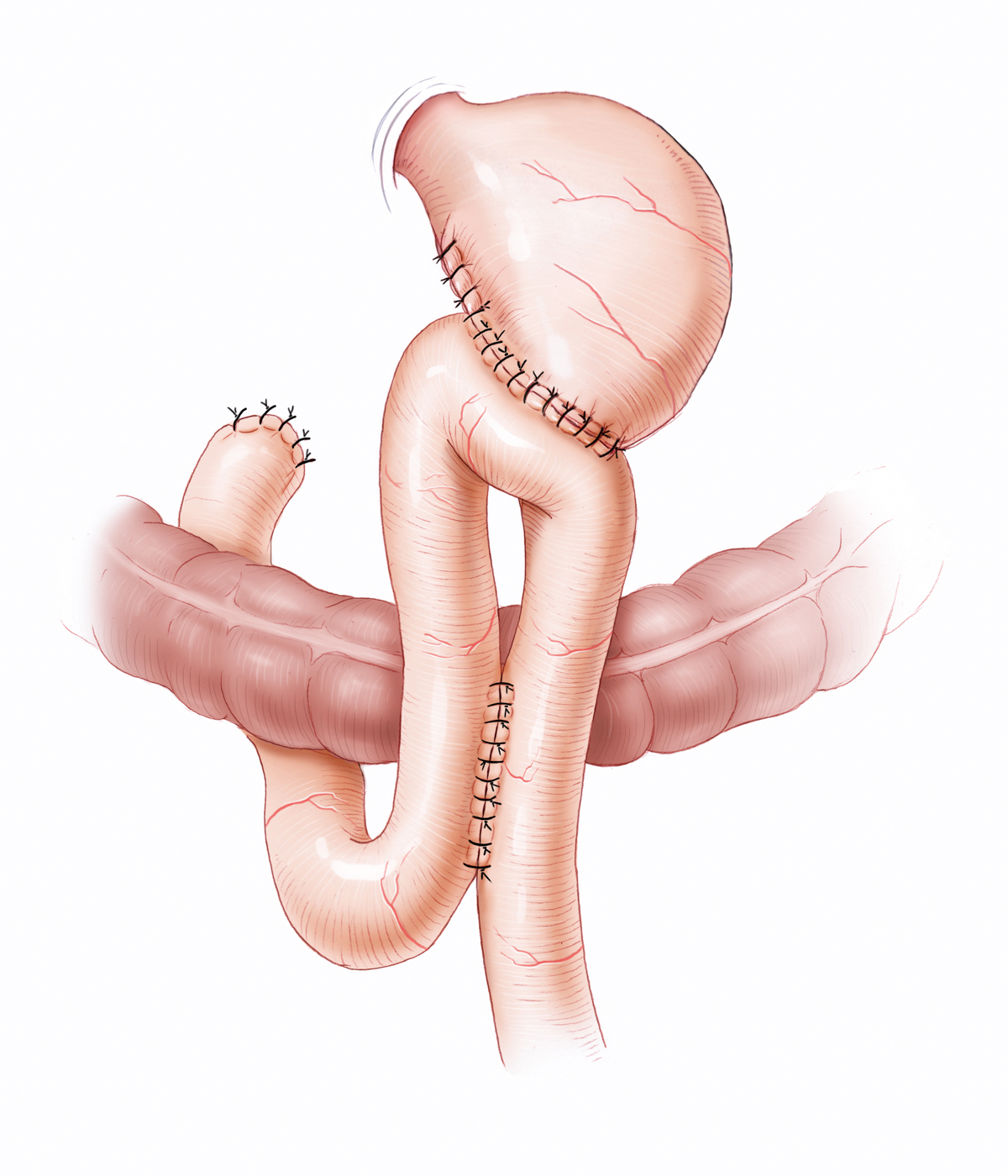
Reconstruction can be done with or without preservation of the duodenal passage. Operation types Billroth I and Billroth II are differentiated. In Billroth I a gastroduodenostomy is performed, the digestive tract remains intact except for the resected antrum segment with pylorus. In Billroth II, the duodenum is sewn closed, the alimentary canal is reconstructed by gastrojejunostomy. Here it is possible to attach laterally by suture a loop of the small bowel and to create a bypass connection at the end-to-side attachment point of the loop between the limbs. This Braun anastomosis prevents reflux of bile into the stomach. Alternative reconstruction can be done according to Y-Roux, in which the biliopancreatic loop is sutured laterally to the efferent alimentary loop.
In emergency surgery for a perforated ulcer or a bleeding ulcer refractive to therapy, it is sufficient to excise the ulcer with a safe resection margin and examine it histologically. Partial gastric resection is limited to patients who do not respond adequately to conservative therapy.
Therapy – Duodenal Ulcer
In duodenal ulcers, the cause of the ulcer and the site of its manifestation are separated. Moreover, concordant malignancies are extremely rare and duodenal resection associated with higher morbidity. The operative therapy of choice for duodenal ulcers is therefore partial denervation of the stomach. In selective proximal or proximal-gastric vagotomy, the vagus nerve fibers supplying the acid-producing portions of the stomach are selectively severed, preserving the motor nerve fibers to the gastric antrum important for gastric emptying.
In emergency surgery for perforation or therapy-refractive bleeding, a duodenotomy is performed and the supplying vessel ligated by stitches. Especially when treating ulcers located on the posterior wall the anatomy be taken into account, and the fact that anastomoses are present in the area supplied by the gastroduodenal and superior mesenteric arteries, which makes it necessary to oversew the supplying vessels on both sides of the ulcer. Otherwise there is a high risk of recurrent bleeding. In operations near the pylorus, a pyeloplasty, i.e. widening of the pylorus, should always be performed to avoid the risk of a gastric emptying disorder.
Postoperative Problems
Dumping Syndrome
Removal of the pylorus and/or partial denervation of the stomach change the emptying of the stomach. Accelerated passage of the food through the intestine can lead to so-called dumping syndrome. An early and a late form are distinguished. Early dumping occurs when hyperosmolar contents pass too rapidly into the small intestine. In accordance with the osmotic gradient, fluid flows from the plasma into the small intestine, leading to diarrhea, cramping, circulatory disorders, dizziness, and profuse sweating. Late dumping is characterized by reactive hyperglycemia accompanied by a rapid drop in blood glucose levels. This usually occurs 60 to 90 minutes postprandial.
Gastric Stump Carcinoma
A frequent sequel of partial gastric resection is atrophic gastritis, which occurs 5 to 10 years postoperative. It can favor the development of a gastric stump carcinoma.
Malnutrition, Malabsorption, Anemia
An altered sensation of hunger and reduced stomach volume lead to diminished food intake. These reconstruction related changes can further impair resorption. The absence or reduction of gastric intrinsic factor, which is produced by parietal cells of the stomach, means that vitamin B12 can no longer be sufficiently absorbed in the terminal ileum with consequent macrocytic hyperchromic anemia.
Afferent/Efferent Loop Syndromes
A stenosis in the afferent loop causes the retention of bile, which can suddenly empty into the stomach and lead to bilious vomiting, after which the patient experiences an immediate improvement in the cramp-like, right-sided epigastric pain. This is termed afferent loop syndrome. In efferent loop syndrome, the stenosis in the efferent loop causes retention of the stomach contents, which again can lead to vomiting.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma