Hemorrhoids
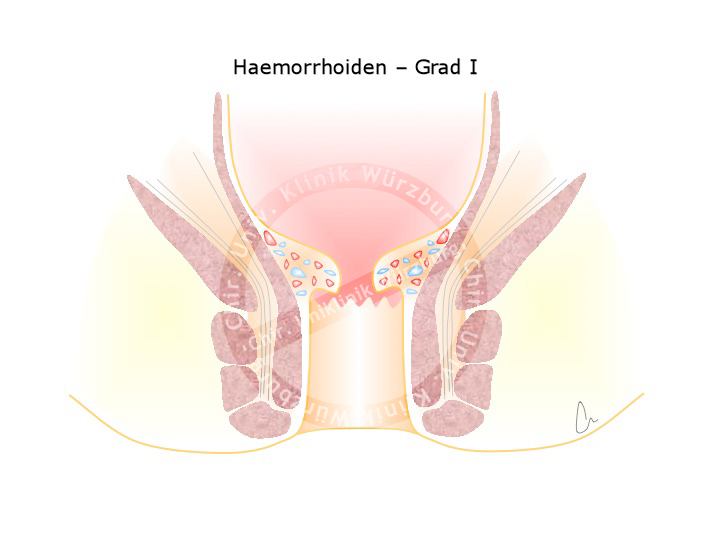
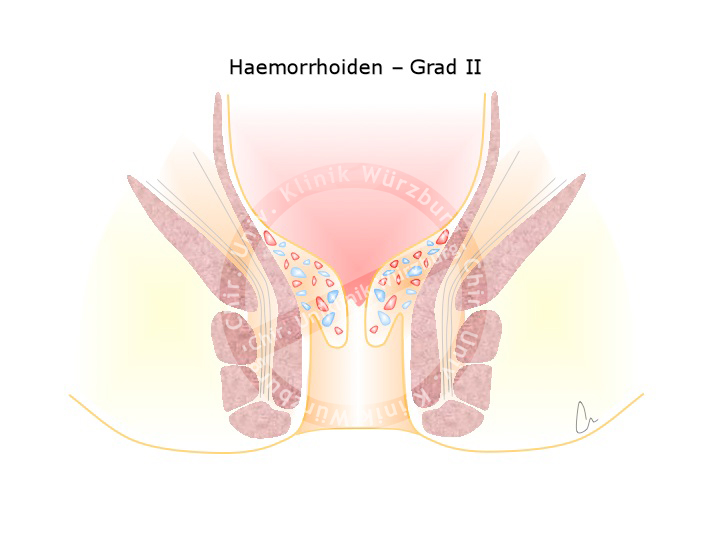
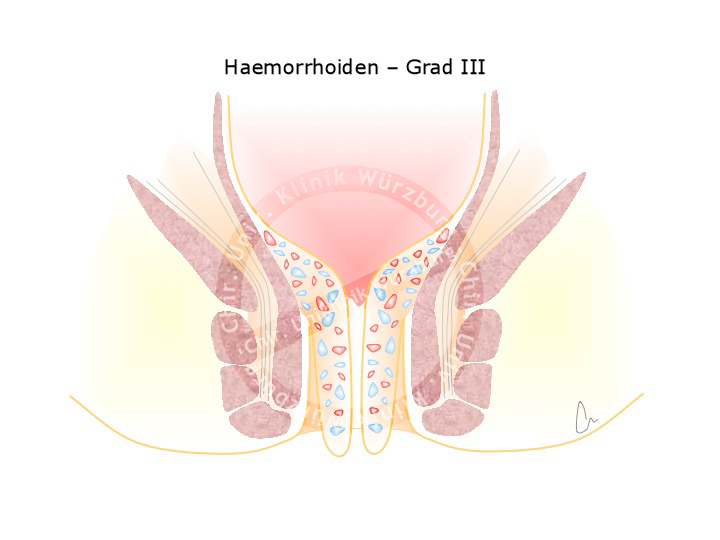
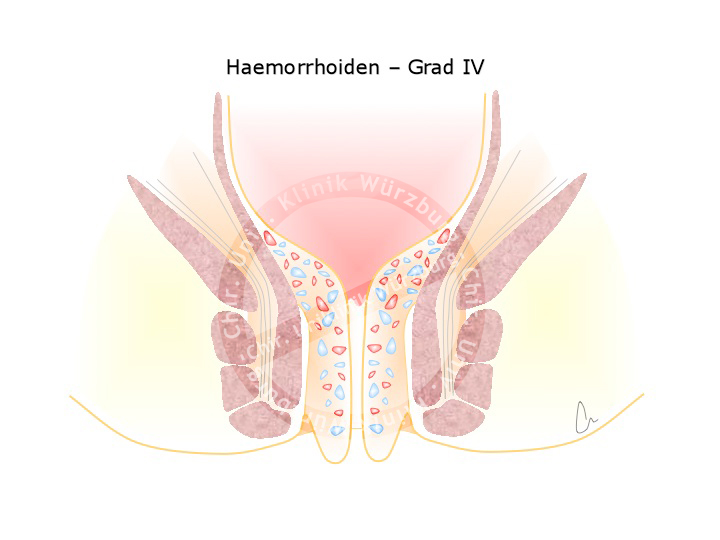
A plexus of veins and arteries helps to seal the anal canal, preventing the leakage of fluid or gas. This hemorrhoidal plexus is present in every person and important for the regulation of fine continence. Enlargement of this vascular plexus due to high pressure e.g. during difficult bowel movement gives rise to grades II, III or even IV hemorrhoids. Grade II hemorrhoids are enlarged at the site, prolapse through the anus upon pressing, and reposition spontaneously. Grade III hemorrhoids can be repositioned manually, grade IV cannot.
Hemorrhoids are caused by a disturbance of the fine continence, with leakage from the anal canal causing a characteristic burning sensation, itching, and wetting. Mechanical irritation can also lead to bleeding, typically seen as a bright red deposit on toilette paper. Hemorrhoids are usually not painful, only if they are so large they protrude from the anal canal do they cause pain.
Therapy
Diagnosis is based on a typical medical history and corresponding proctoscopy finding. If there is perianal bleeding, however, it is not enough to be satisfied with the diagnosis of hemorrhoids, sources of bleeding higher up in the colon must be excluded by e.g. colonoscopy.
Treatment of hemorrhoids consists of sclerotherapy or strangulation with elastic bands for stage II hemorrhoids. For stages III and IV a hemorrhoidectomy is performed, where the hemorrhoids are discretely dissected while preserving the sphincter muscle apparatus and the supplying artery is ligated.
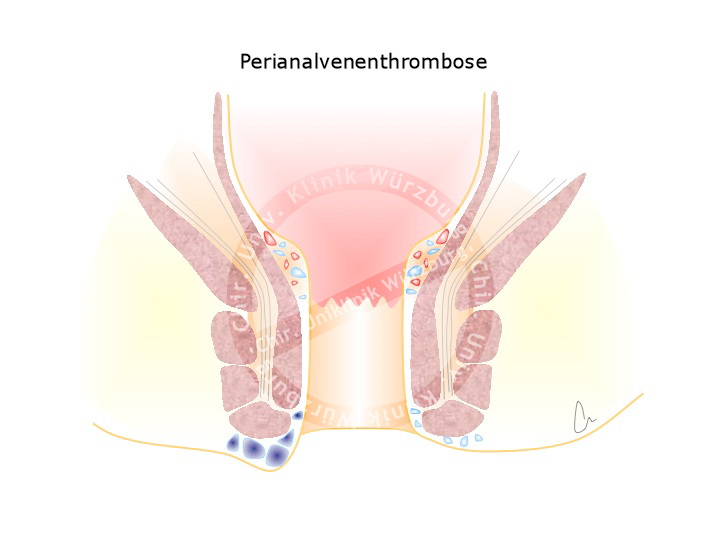
Hemorrhoids are to be distinguished from perianal venous thromboses, which are often erroneously termed exterior hemorrhoids. A perianal venous thrombosis is a thrombosis of the perianal veins unrelated to the hemorrhoidal plexus. This acute and painful clinical picture can be caused by powerful pressing, e.g. during childbirth. In the acute phase, the thrombosis can be incised under local anesthesia and expressed. If left untreated, the pain subsides after a few days and the thrombosis resolves over time, with possible adjuvant application of an heparin-containing ointment. As residuum a skin fold usually remains, a so-called Marikse.
Anal Fissure
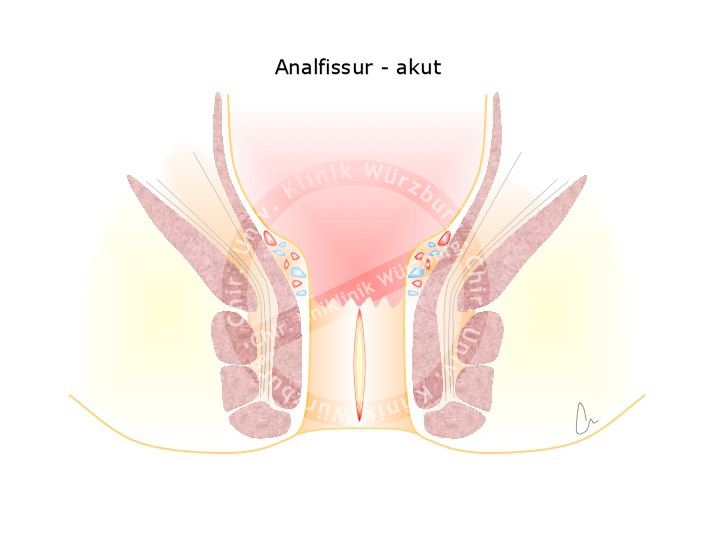
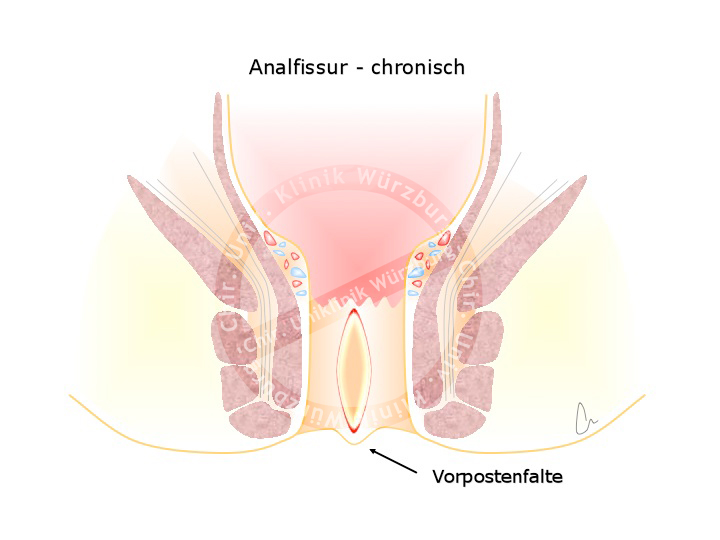
Anal fissures are very painful and associated with bleeding. They arise when hard stool causes a mucosal tear in the anoderm. Unlike the rectum, the anoderm is highly sensitive to pain. Patients with anal fissures report an intense burning sensation and pain during and after bowel movements as well as bloody deposits on the stool and toilette paper.
The pain causes a reflexive tensing of the sphincter apparatus, which worsens the bleeding in the area of the fissure and thus impedes the healing process.
Treatment attempts to lessen the sphincter spasm by applying e.g. nitrate or calcium channel antagonists to improve anal perfusion. New anal fissures usually heal in this manner, while older chronic fissures are often bordered by heaped up scarred tissue that impedes healing. Chronic fissure may require subtle resection of the fissure and notching of the underlying hypertrophied local sphincter. This resembles treatment of an incisional wound which after more than 6 h to 8 h can no longer heal despite suturing and must be cut out.
Abscesses and Fistulas
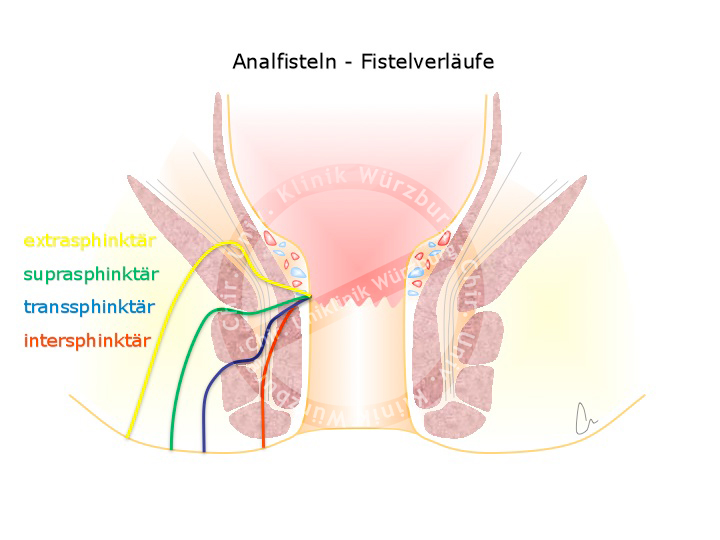
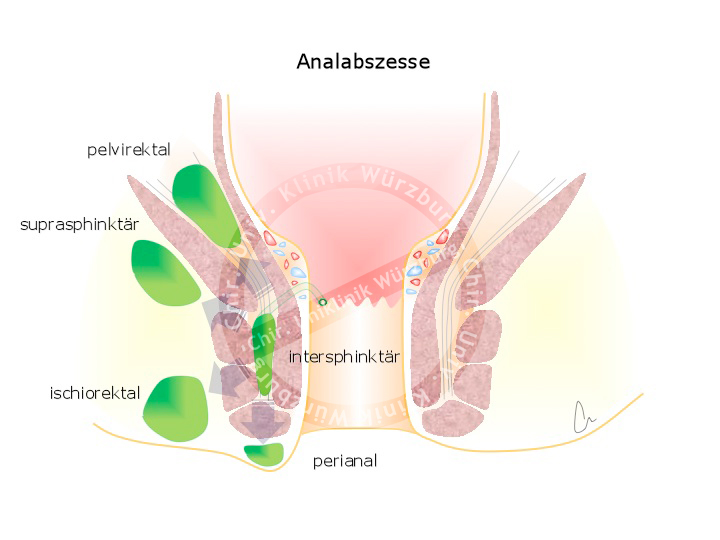
A fistula is an unnatural connection between two hollow organs or between a hollow organ and the skin. A perianal fistula is a connection between the anal canal or the rectum and the skin. These fistulas usually arise from an inflammation of the proctodeal glands, which are located between the external and internal anal sphincters comprising the sphincter muscle apparatus and the excretory ducts of the anal glands.
The pus that forms in inflammation can infiltrate through the sphincter muscle into the fat tissue surrounding the anus. The acute form of an anal fistula is the perianal abscess, the chronic form is fistula itself. Fistulas can also form in the context of chronic inflammatory bowel diseases, chiefly Crohn’s disease.
Symptoms
A perianal abscess is accompanied by pain, swelling, and redness of the surrounding tissue. Fever may also occur. Lancing and draining of the abscess outwards relieves the symptoms. A fistula usually does not cause severe complaints, patients do however report persistent secretion that causes itching and a burning sensation.
Diagnosis
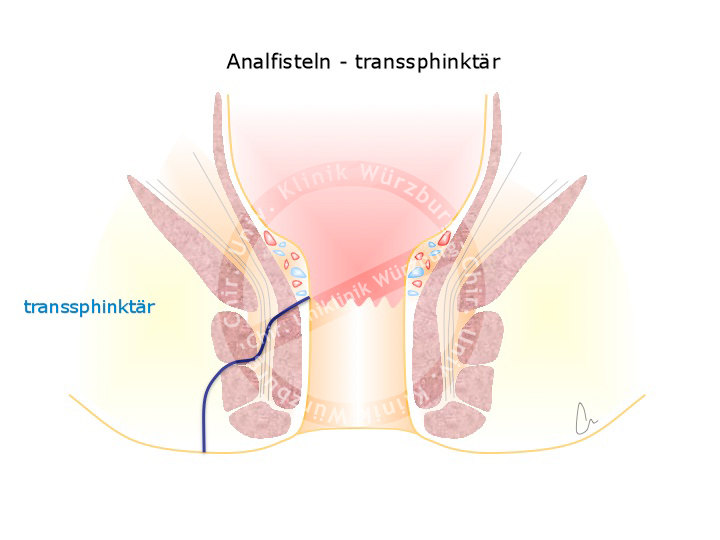
The tract of a fistula can be shown by endosonography. Fistulas can be classified according to their tract through the sphincter muscle apparatus. In the Parks classification fistulas are classified into four types: inter-sphincteric (~70%), trans-sphincteric (25%), supra-sphincteric (5%), and extra-sphincteric (1%). These are to be distinguished from pilonidal cysts, which are often incorrectly called sacrococcygeal fistula. Anatomically they are not fistulas because they do not connect with a hollow organ. They are rather an inflammation of ingrown hair in the anal cleft.
Therapy
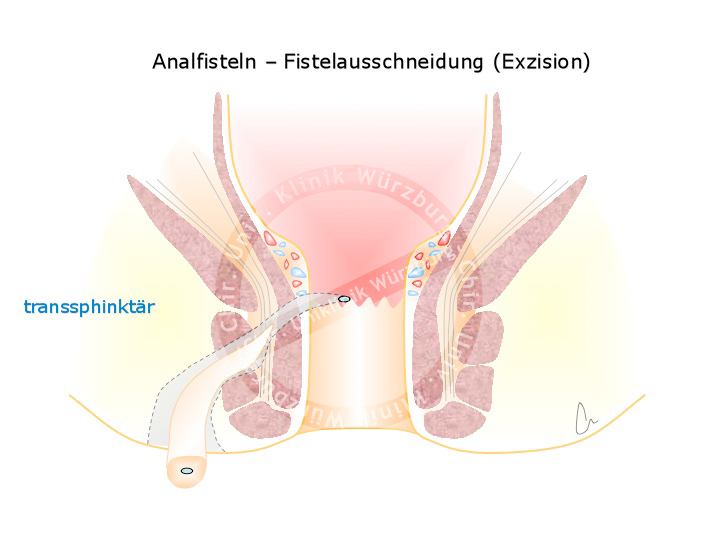
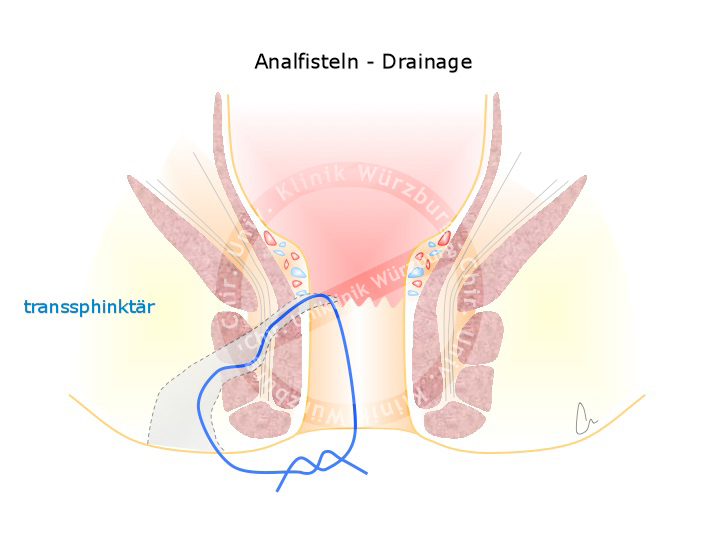
The goal of surgery is to remove the inflammation from the area of the sphincter muscle without injuring the muscle. This requires a two part strategy. In the first part, the abscess is subtly excised and the fistula marked with a rubber loop. This ensures that the fistula does not completely adhere, which could result in recurrence of the abscess. When the abscess has completely subsided, the second part definitively treats the fistula. Depending on the fistula’s tract through the sphincter, the fistula is simply cut open or it is covered with a flap-plasty. Another option is placement of an anal fistula plug, which involves pulling a cone-shaped cellular matrix plug into the fistula tract to serve as a matrix for host cell remodeling.
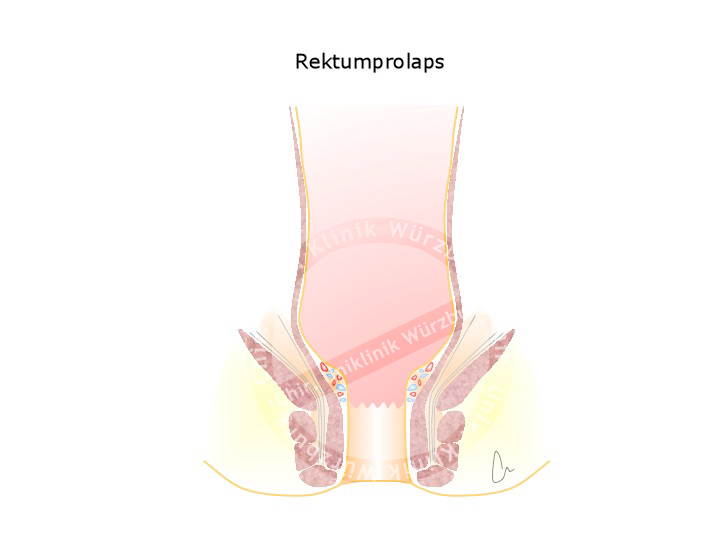
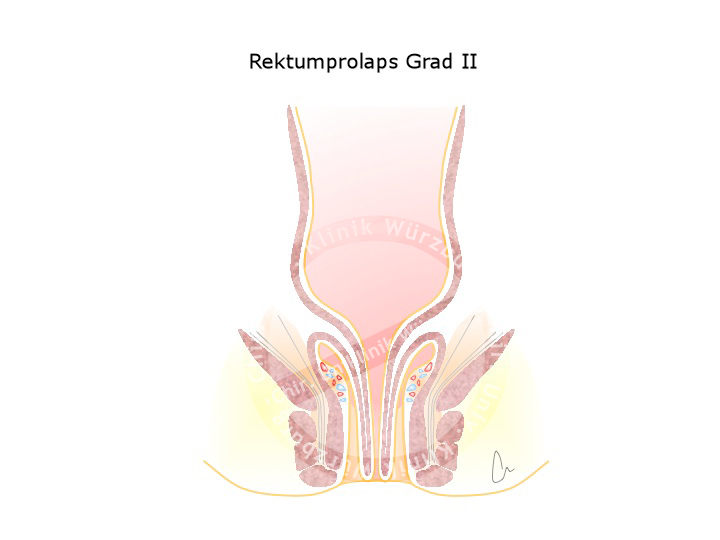
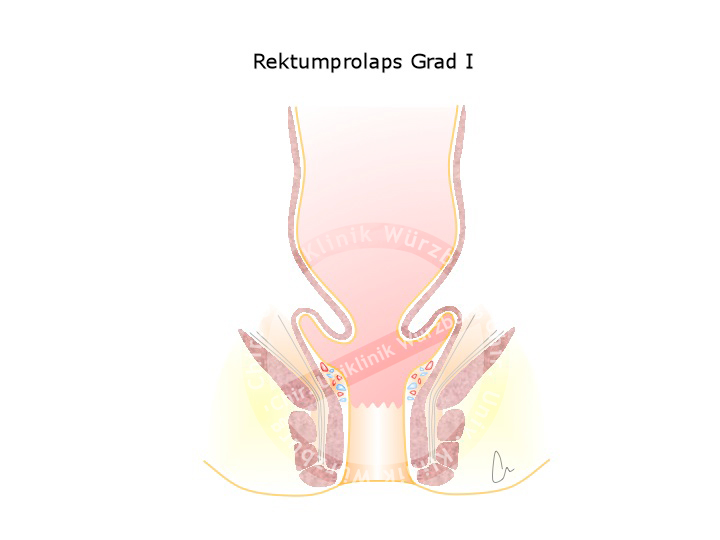
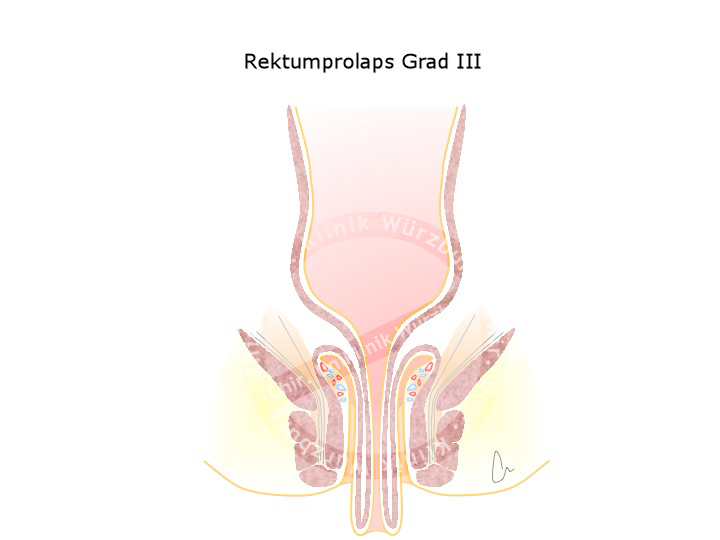
Rectal Prolapse
A weakness in the pelvic floor can result in the wall of the rectum protruding out of the anus. This rectal prolapse has various grades of severity. Females are affected much more often, especially if they have given vaginal birth to multiple children.
Rectal prolapse is to be distinguished from anal prolapse, which corresponds to third or fourth grade hemorrhoids. An anal prolapse exhibits radial folds, a rectal prolapse circular folds.
Therapy
In addition to conservative measures like stool regulation, there is a general indication for surgery. A transabdominal access can be chosen and the rectum stitched to the pelvic wall, a procedure called rectopexy. If during the procedure the elongated bowel is also shortened, one speaks of a resection rectopexy.
Another surgical procedure that shortens the bowel from transanal is the Altemeier procedure for rectal prolapse. Here the prolapsing part of the rectum is resected in lithotomy position and the two stumps joined in a coloanal anastomosis.
Constipation & Incontinence
Die anale Inkontinenz kann ihre Ursache in einer Störung der Schließmuskelfunktion haben, die beispielsweise durch eine traumatische Entbindung entstanden ist. Die anale Endosonografie kann Sphinkterdefekte zuverlässig darstellen. Im Einzelfall kann eine operative Rekonstruktion des Schließmuskelapparates helfen.
Bei älteren Frauen und oft nach einer Hysterektomie oder mehreren vaginalen Entbindungen kommt es zu Veränderungen des Beckenbodens, die sowohl eine Inkontinenz auslösen können als auch Schwierigkeiten bei der Stuhlentleerung verursachen können. Dieses sog. Obstruktive Defäkationssyndrom (ODS) ist ein komplexes Krankheitsbild, das einer differenzierte Diagnostik und Therapie bedarf.
Durch das Entfernen des Uterus entsteht eine Lücke im Beckenboden, die ein Tiefertreten des Dünndarms ermöglicht und zu einer inneren Abknickung des Rektums führen kann. Man spricht in diesem Fall von einer Enterozele oder einer Intussuszeption. Die Harnblase kann sich ebenso als Enterozele in den Beckenboden absenken und die Defäkation erschweren. Meistens kommt es noch zu einer Aussackung des Rektums nach ventral, einer Rektozele, in der sich beim Entleerungsversuch der Stuhl sammelt und zum Gefühl der unvollständigen Entleerung führt. Oftmals ist eine Entleerung ohne Hilfsmittel nicht mehr möglich.
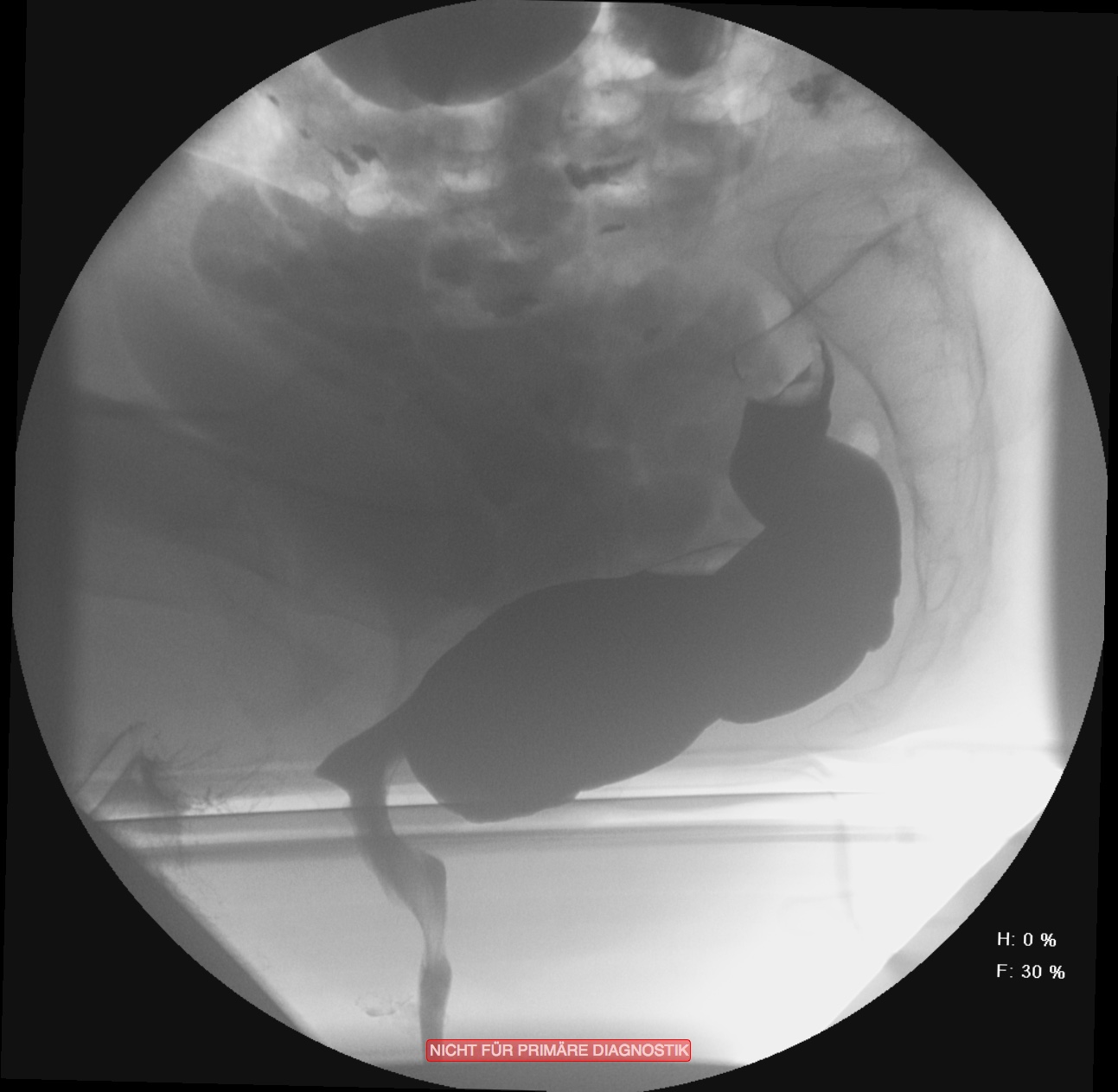
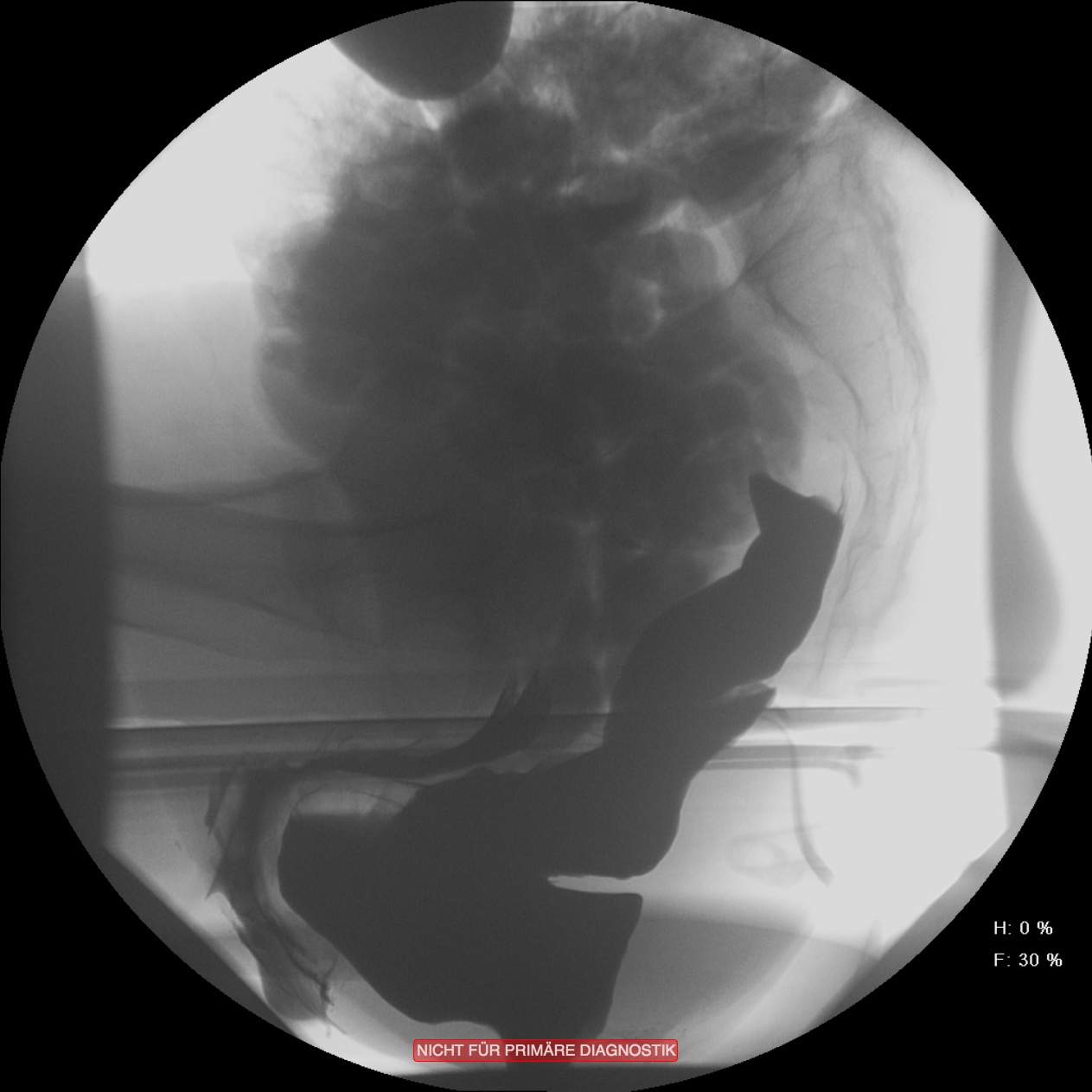
In vielen Fällen ist diese Obstruktion mit einer gleichzeitig bestehenden Inkontinenz kombiniert. Dies erscheint auf den ersten Blick etwas paradox. Durch die andauernde unvollständige Entleerung ist die Rektumampulle aber nie vollständig geleert und der Schließmuskelapparat durch die ständige Überdehnung des Beckenbodens nicht in der Lage, den Stuhlgang immer suffizient zurückzuhalten. Zur Differentialdiagnostik werden Sphinktermanometrie, Endosonografie, Rektoskopie und ein Röntgenverfahren, die Defäkografie angewendet. Diese erlaubt eine Darstellung der funktionellen Abläufe und anatomischen Veränderungen während der Defäkation. Das Ausmaß der Obstruktion und der Inkontinenz wird mit anamenstischen Score-Werten objektiviert.
Therapy
Therapy is directed at the type of disorder. It may, for example, comprise a full wall resection of the rectum to eliminate the internal prolapse of the bowel that prevents defecation. In some patients, the incontinence worsens after such an operation, so that a pacemaker-like device must be used to aid sphincter control. This device stimulates the sacral nerves where they leave the sacrum to increase the contractile force of the sphincter muscles.




 Wound Healing
Wound Healing Infection
Infection Acute Abdomen
Acute Abdomen Abdominal trauma
Abdominal trauma Ileus
Ileus Hernia
Hernia Benign Struma
Benign Struma Thyroid Carcinoma
Thyroid Carcinoma Hyperparathyroidism
Hyperparathyroidism Hyperthyreosis
Hyperthyreosis Adrenal Gland Tumors
Adrenal Gland Tumors Achalasia
Achalasia Esophageal Carcinoma
Esophageal Carcinoma Esophageal Diverticulum
Esophageal Diverticulum Esophageal Perforation
Esophageal Perforation Corrosive Esophagitis
Corrosive Esophagitis Gastric Carcinoma
Gastric Carcinoma Peptic Ulcer Disease
Peptic Ulcer Disease GERD
GERD Bariatric Surgery
Bariatric Surgery CIBD
CIBD Divertikulitis
Divertikulitis Colon Carcinoma
Colon Carcinoma Proktology
Proktology Rectal Carcinoma
Rectal Carcinoma Anatomy
Anatomy Ikterus
Ikterus Cholezystolithiais
Cholezystolithiais Benign Liver Lesions
Benign Liver Lesions Malignant Liver Leasions
Malignant Liver Leasions Pancreatitis
Pancreatitis Pancreatic carcinoma
Pancreatic carcinoma